The challenge for health services in the UK is to create capacity in the community for the increasing number of older people, so that they can be cared for close to home. Local community hospitals attract strong support from their communities and are successfully extending their role to meet increasing needs.
The new Chief Executive of NHS England, Simon Stevens, has announced that he believes that ‘small hospitals have a big part to play, especially for older people’. This statement signals a shift in emphasis from a centralised and highly specialised service towards a more local, generalised and holistic service. The National Health Service in the UK is responding to changes in the population and its health needs by recognising the increase in older people who are typically frail, have comorbidities and complex care needs, and who require both health and social care. Where possible, the NHS aims to care for patients in their own homes or close to home facilities such as community hospitals rather than in specialist, acute care hospitals.
Community Hospital Services
The 450 community hospitals in the UK are well placed to provide many of the required local services. Originally called ‘cottage hospitals,’ they were created to provide a safe and clean environment of hospital beds for the treatment of patients living in rural and remote areas.They have expanded their original service scope and have diversified with many of them now offering extended services and facilities to meet a wide range of health and social care needs.
Community hospitals are described as small local hospitals serving a defined population. Most of the facilities have less than 30 beds but the range varies from 10 to 100 beds. The hospitals have nurse-led services with medical support provided by local family doctors. There are no resident doctors. Community-based staff have direct access to services, unlike the system with acute care hospitals that operates by ‘referral only’.
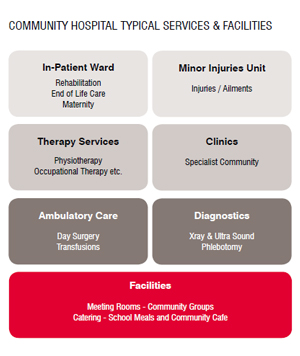
The community hospital is often described as a health and social care ‘hub,’ where many different healthcare providers deliver services. There is a wide variation of services in community hospitals, but key service areas include in-patient care, clinics, minor injuries units, diagnostics, therapy services and ambulatory care.
Community hospitals offer community beds that are not designated to any speciality but are used according to need. Patients can be admitted for inpatient care such as rehabilitation, assessment, sub-acute care or end of life care. Patients, on an average, stay for around two weeks, although assessment may just require a short stay and patients with complex rehabilitation may need to stay longer. The in-patient beds offer intermediate care, and help achieve the ambition of reducing unnecessary admissions to specialist District General Hospitals (DGHs). Research on intermediate care in the community hospitals has demonstrated the care to be appropriate, effective and associated with greater independence. In particular, post-acute rehabilitation at community hospitals has been assessed as cost-effective and is appreciated by patients.
 Community hospitals are now offering a range of clinics such as rapid access clinics for older people, audiology, rheumatology, mental health services and many more. It has been shown that the availability of clinics such as rapid access clinics help reduce admissions to hospital, resulting in only 15 per cent of patients seen in the clinic being admitted to a DGH. ‘One stop clinics’ are also offered, where practitioners concerned with a particular condition or illness work together with feasible clinic times for patients so that they may be seen by different practitioners as required in one visit. A diabetic one-stop clinic would include a consultant physician, a diabetic specialist nurse, a podiatrist or chiropodist, an ophthalmologist and a dietician. This integrated way of working has proved to be effective for the patient and for the service providers.
Community hospitals are now offering a range of clinics such as rapid access clinics for older people, audiology, rheumatology, mental health services and many more. It has been shown that the availability of clinics such as rapid access clinics help reduce admissions to hospital, resulting in only 15 per cent of patients seen in the clinic being admitted to a DGH. ‘One stop clinics’ are also offered, where practitioners concerned with a particular condition or illness work together with feasible clinic times for patients so that they may be seen by different practitioners as required in one visit. A diabetic one-stop clinic would include a consultant physician, a diabetic specialist nurse, a podiatrist or chiropodist, an ophthalmologist and a dietician. This integrated way of working has proved to be effective for the patient and for the service providers.
Most community hospitals have ‘minor injuries’ units, some of which also attend to minor ailments. These offer swift access to clinical assessment followed by treatment, referral or discharge. In some areas these services are being expanded in order to try and relieve the workload and pressure on the emergency departments in DGHs.
The diagnostic services usually include X-ray, ultrasound and phlebotomy. Some hospitals offer CT scanning and may offer day procedures such as gastroscopies. Ambulatory services also include blood transfusions and intravenous treatments. A number of community hospitals have services such as maternity, kidney dialysis and day surgery. Services for older people include memory clinics and dementia care units.
The range and scope of the service provision continues to expand beyond healthcare offering social, welfare, leisure and wellbeing services. Their role in health education, health promotion and involvement in the wider community through work in schools, colleges and public services, has led them to being described as part of the social fabric of their community.
Characteristics
Three of the key characteristics of the community hospital model are described below: local medical care, integrated working and support from the local communities.
A feature of community hospital care is the role played by local family doctors. Local family doctors work in the hospital offering intermediate care, which is described as a bridge between primary care (general practice) and secondary care (DGH). GPs work as part of a formal multi-disciplinary team with nurses, physiotherapists, occupational therapists and social workers, with additional practitioners invited to join as required.
Joint working is a strong feature of the community hospital model. A study on ‘joint working’ across disciplines, sectors services and staff demonstrates that services are provided through partnerships. Partnerships that were particularly evident were those between the community hospital other health sectors (primary and secondary care), and agencies (third sector, social services and councils). Integrated care is a global priority in healthcare. The study shows that community hospitals can provide evidence of a long tradition of a long tradition of integrated working for patients of all ages and conditions.
Another feature of the community hospital model is the level of involvement and support from local people. Community hospitals were created through public donations of land and finance, and have a long tradition of providing care for over 100 years. Each hospital has an organised group of local people known as the League of Hospital Friends who support the hospital through activities such as fund raising and organising volunteers to work with the hospital. Funds are used for overall patient benefit, and for equipment furnishing, staff training and improvements to buildings. Local people are fiercely loyal to their local hospitals, and demonstrate it through highly active campaigns if there is any suggestion of reducing or closing services.
Improving Care for Older People
Older people express satisfaction with the service, and cite features such as a high quality care that they can trust, including accessibility, familiarity of the hospital and staff and continuity of care.
Community hospitals can help improve care for older people by providing a service that they can be confident about, knowing it can offer a range of services to meet their changing needs. The community hospital often has a good reputation, and has been trusted by its community over many years. The tradition of care over generations is deemed important and local communities often speak of trusting the quality of care at ‘their’ hospital. This sense of ownership is a feature, and is visible in many aspects of the way the hospital operates.
Community hospitals are more domestic in size and scale than the specialist centralised acute hospitals, and are therefore less daunting and disorientating than large hospitals with long corridors and multiple clinical spaces. Patients, when asked, value the fact that the hospital is close to home, they can park easily and it is accessible for patients and visitors alike. For patients who are frail and vulnerable, and who may have compromised mobility and cognitive limitations, these considerations are important.
Patients value the fact that they are being cared for by staff that they know. Community nurses and therapists provide home-based care as well as care within the hospital, and so patients may see familiar staff who live locally, including their own family doctor.
It is known that older people appreciate being cared for by those who already know them, and know not only their medical conditions but also their social circumstances. This has been referred to as holistic care by staff, and complies with the person-centred care approach.
Patients can be supported in their local hospital throughout the progression of recovering from an illness, condition or from an incident or intervention such as an operation. The model of care ranges from helping patients to retain or maintain their independence, while supporting those who are living with long term conditions; monitoring and supporting those with deteriorating conditions and life threatening illnesses, and also patients requiring palliative care and end of life care. There is a challenge for staff working in small hospitals with such a wide remit which requires a wide range of skills, although clinical support and training is provided to generalist staff by specialist nurses and consultants.
Shared Learning
The Community Hospitals Association (CHA) for England and Wales supports staff and organisations that are providing community hospital services by developing a network of members for sharing good practice, offering advice and promoting community hospitals. The CHA is working with research institutions to further develop an evidence base to support informed decision-making for the future of community hospitals.
Community hospitals were originally established in the UK over 100 years ago. Over time many of the original hospital buildings have been extended, redeveloped or replaced in order to meet required clinical and quality standards. However there are still community hospitals that require financial investment in buildings and this represents a challenge. Providers of community hospitals also face challenges in managing complex contractual arrangements for services, involving multiple partners. The partnership model has helped to create some innovative developments however, such as with social care and housing.
The model of the community hospital can be found outside of the UK, such as in Norway and the first community hospital in the Netherlands. This demonstrates that features of the model may be replicated elsewhere, adapted and located within other health systems.
Conclusion
In summary, community hospitals in the UK have been providing care that is person-centred, integrated, and highly valued by the communities they serve. There is evidence of effective care for older people, particularly with outcomes for rehabilitation.Studies show that savings can be made for the health economy by providing more care locally. With an increasingly ageing population such local services will become more important and valued.The service therefore not only meets national health policy, but it also fulfils the needs of patients, care providers and their communities.
1. Local Care
 Mr Smith, aged 85 years was transferred to his local community hospital after he had spent a day in a very busy assessment ward in a DGH, 35 miles away. He was assessed as he had a fall and was immobile and confused. He was diagnosed with urinary infection and had a history of prostate cancer. He arrived in the evening, exhausted, confused, dehydrated and unable to move. He agreed on his plan of care, and after several days of medication, nutrition, physiotherapy and occupational therapy and nursing care, he declared that he felt like a new man and is now able to walk across the room. He said that only when he got to his local hospital could he start to recover. He appreciated having his own doctor looking after him. He also said that it helped his wife visit him as he was close to home.
Mr Smith, aged 85 years was transferred to his local community hospital after he had spent a day in a very busy assessment ward in a DGH, 35 miles away. He was assessed as he had a fall and was immobile and confused. He was diagnosed with urinary infection and had a history of prostate cancer. He arrived in the evening, exhausted, confused, dehydrated and unable to move. He agreed on his plan of care, and after several days of medication, nutrition, physiotherapy and occupational therapy and nursing care, he declared that he felt like a new man and is now able to walk across the room. He said that only when he got to his local hospital could he start to recover. He appreciated having his own doctor looking after him. He also said that it helped his wife visit him as he was close to home.
2. Community Initiative
A group of volunteers for the community hospital who were members of the League of Hospital Friends were concerned about the high incidence of hip fractures in older people in their town. They consulted the GPs, and decided to purchase a dexa scanner for the hospital to enable early detection of osteoporosis. The group also funded staff training and support. They talked to GP practice staff and local groups, promoted the service and supported auditing of the service.
3. Life Stories
A community hospital day unit provided support for older people including those with dementia. Staff wanted to create a project that would help older people to remember and celebrate their lives. They decided to encourage school children to offer to work with patients to create their ‘life stories.’ The resulting life stories were presentations illustrated with photographs and the patient’s favourite music. This intergenerational project is a feature of the local hospital being part of the community and was granted an ‘Innovation and Best Practice Award’ by the Community Hospitals Association.
References