The growing number of COVID-19 infections worldwide are confronting healthcare institutions around the world with unprecedented clinical and operational challenges pushing many of them to their limits and putting the issue of health into sharp focus for all of us. Many of the already existing challenges such as access to care or shortage of qualified staff, have been further intensified by the pandemic. In this interview, Elisabeth Staudinger explains the role of digital solutions in care delivery and how the current pandemic is accelerating the efforts of digitalising healthcare.
Even before the pandemic, digital solutions had started to penetrate our daily lives. Online shopping made our lives more convenient. Navigation systems made our car ride more efficient by avoiding areas of increased traffic. Our watches told us how we were keeping up with our fitness goals. Today, connecting care teams and patients has become easier than ever before and making decisions based on data is easing the workload of care providers and enabling more accurate diagnoses. In fact, even before the pandemic, 9 out of 10 physicians saw the benefits of virtual care technologies1. The pandemic has accelerated the adaptation of digital means. For healthcare, that’s good news. Digital solutions will enable healthcare providers to deliver higher value care and tackle the challenge of providing access to care in this region.
Improving access to care is one of the most pressing challenges in many countries in Asia. While countries such as Australia and Japan are ranked 4th and 8th respectively in the Global Access to Healthcare Index, others such as the Philippines, Indonesia, Vietnam and India still have much room for improvement with their ranks ranging from 35th to 45th position2. Those living on distant islands, remote mountains or rural regions face even harder challenges than those living in the cities. Ironically, the fewest healthcare professionals are usually found where the health needs are greatest, the so-called “inverse care law” in healthcare. In addition, in 2014 countries in South Asia spent on average just US$67 per capita on health – significantly lower than the OECD average of US$4,7353. At the same time, the Asia-Pacific region has the highest level of dependence on out-of-pocket expenditure of any region according to the World Health Organization (WHO) and the highest number of households driven into poverty in order to pay for healthcare4.
Improving access to care means making care more affordable, available and accepted by the population. Affordability means that patients can ‘consume' or use health services such as state-of-the-art diagnostics and treatment without causing financial hardship. Availability means that healthcare services are there when and where they are needed, in particular, close to the patients. Finally, accepted means helping populations to understand the value of care and utilise their care options.
During the pandemic, even countries with the best healthcare systems struggled. Availability became a challenge as most resources were shifted to care for COVID-19 patients. Even patients who usually would have had access to care were suddenly left with none or very little. Outpatient services, elective procedures and non-emergency cases were put on hold. Access became more difficult with limited transportation or higher cost of travel due to social distancing. As financial struggles grew among the poor, healthcare became even more unaffordable. Yet, others may have actively chosen not to utilise care options either to stay away from the potential risk of infection or because they could not justify a visit during the crisis. The result is an increased disease burden. In fact, delaying treatments can have lasting consequences. For example, in breast cancer patients, delaying treatment from two weeks to more than six weeks can lower the five-year survival rate by as much as 10 per cent5.
The vision for healthcare is to keep people as healthy as possible and that requires people to be able to access care. More than ever, the efforts of MedTech players like Siemens Healthineers need to be geared towards improving access to healthcare in many parts of the world, and especially in Asia.
During the pandemic, people started seeking ways to obtain care from home for the reasons mentioned above. First, digitalisation made inroads in the self-assessment of COVID-19 symptoms. Second, we have seen providers ramping up their telemedicine capabilities and recruiting more doctors faster than ever. These services connect healthcare providers and patients though virtual platforms. Third, various digital solutions are being developed in the area of home monitoring to support the patient, monitor vitals and provide alerts. Bendigo Health became one of the first hospitals in Australia to roll-out telemonitoring in the fight against COVID-19. Our digital care application supplies doctors and nurses with a dashboard of daily updated symptoms and health vitals to remotely stay on top of their patients
health.
Governments play a vital role in accelerating the adoption of such technologies. In Indonesia, for example, the Ministry of Health partnered with ride-hailing technology firm Gojek and telemedicine provider Halodoc to offer quick online consultations for those experiencing COVID-19 symptoms. South Korea eased restrictionson telemedicine to treat COVID-19 patients remotely, while Japan launched a free governmentsupported remote health consultation. Australia extended Medicare coverage for telemedicine consultations.
In essence, digital solutions can provide better access and triage patients, starting as ‘digital front door’ and – depending on the condition – continuing with the provision of health services, such as telehealth. In doing so, we can keep non-urgent patients away from the hospitals that are overloaded, and patients can get care in the comfort of their home, avoiding travel, cost, waiting times and the potential risk of infections. In short, by creating ways to connect care teams and patients we can make healthcare delivery more efficient.
The lack of skilled healthcare professionals became painfully obvious during the pandemic. Despite all efforts to attract, train and retain healthcare professionals, the WHO projects a global deficit of about 12.9 million skilled health professionals globally by 2035. In South-East Asia, the absolute deficit is projected to be 5 million and thus highest in the world – representing 39 per cent of the global total6. Highly qualified personnel are scarce, and also a relevant cost factor, for hospitals that are already trying to cut costs while keeping quality high. At the same time, most of these health professionals live centrally, making access difficult for the large populations living in distant, remote or rural areas. We must find ways to do more with less and to ease the burden of the overworked healthcare professionals while also extending their reach to farther away locations. There is no healthcare without people to deliver it.
Remote scanning assistance can help in realising this. It helps to make expert knowledge accessible across sites in real time. Technologists can always call on an expert for live support. During the pandemic, such technologies also helped reduce staff exposure to infectious patients. In India, at the Sree Chitra Tirunal Institute for Medical Sciences and Technology, remote scanning assistance has been of immense use during the pandemic. While there are normally three personnel in the console room during an MR exam, only one technologist managed the exam on site, while the other two worked remotely. This not only helped to keep the staff safe
but also required less personal protective equipment which is a scarce resource in current scenario.
Such technologies also help to extend reach. Prachachen Imaging Center (PCC), a leading imaging centre based in Bangkok, Thailand has 17 centres across the country. Normally, their expert radiology team in Bangkok would often travel to these centres, especially for clinical consultation. When an emergency case came in during the lockdown from a centre 500KM away from Bangkok, the experts could make a timely and accurate diagnosis of the patient thanks to remote assistance.
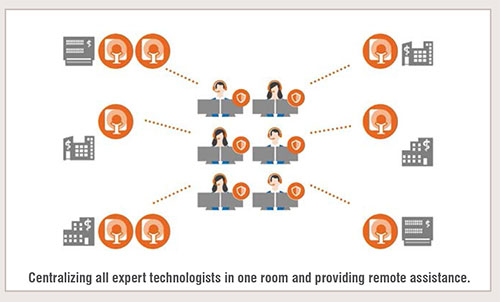
In cancer care, HealthCare Global Enterprises Ltd (HCG) is relying on the hub and spoke model of delivery. Dr. B.S. Ajaikumar, Chairman and CEO of HealthCare Global (HCG), is using this model to take cancer centres to the furthest away places. He has 100 oncologists at the central hub supporting the spokes through telemedicine, tele-radiology, multidisciplinary tumor boards and remote consultation. In addition, during the pandemic, more than 200 oncologists located across the country were providing virtual consultations, too. The clear goal was to ensure consistent, ongoing patient care.
Knowledge sharing is also crucial to keep the quality of care high. Technologies that allow you to share image studies to discuss cases with your peers, even beyond the borders of your own institution are meaningful. It fosters knowledge exchange and research and helps to get the opinion of a more experienced radiologist. By making scarce resources available to more people, we can improve access and quality of care.
To find out more, please click here
Given our lack of skilled professionals, we need to make sure they can allocate most of their scarce time to focus on patients. That means we need to enable them to spend less time on administrative tasks, ease their workload and aid their decision making. Artificial Intelligence (AI) can help remove or minimise time spent on routine, administrative tasks, which can take up to 70 per cent of a healthcare practitioner’s time7. With AI, for example, if you have robust, validated data from one patient, you could compare that to an enormous quantity of data from other comparable patients. We call this clinical decision support. For example, AI applied to CT images can be a useful tool for the detection of COVID-19 symptoms and to help with follow-up and treatment planning. AI-powered analysis of chest scans has the potential to alleviate the workload of radiologists, who must review and prioritise a rising number of patient chest scans.
We will also see decision support for patients or consumers, working in a similar way. Algorithms can assess patients’ needs and prompt them to make lifestyle changes or talk to a care provider in order to better manage—or even prevent—chronic conditions. Healthcare that starts from home is much more efficient than care that starts at a hospital. The later we intervene, the higher the disease burden, requiring more cost and resources.
To find out more, please click here
Asia is at the forefront of digitalisation. In fact, eight Asian nations are in the top 10 when it comes to leading the customer shift to mobile payments, out of which six are in Southeast Asia8.China is leapfrogging the world and has already reinvented ways of accessing primary care and enabling patient self-management as well as expanding telehealth. Access to primary healthcare is a challenge in China, and there is great variability in the quality of care delivered. To cope with this, the Chinese government is investing in Artificial Intelligence (AI). Digital means are already being used to access primary care, to schedule appointments and to triage patients based on AI. Ping An Good Doctor (PAGD) is a good example with its online one-stop healthcare ecosystem in China with over 315 million registered users9. In fact, during the pandemic, their platform recorded 1.1 billion visits with a 10 fold increase in newly registered users and a 9 fold increase in daily consultations10. And they are not the only one – big players like Alibaba and Tencent are also changing the way primary healthcare is delivered.
If we look at India, the government has launched ‘Ayushman Bharat’ – and demonstrated its strong commitment to providing healthcare for all. Several other initiatives such as ‘Digital India’, ‘Start-up India’, ‘Make in India’, are part of the county’s development plan paving the way for improved access to care. With increasing focus on healthcare sector through these initiatives, I am bullish on India’s growth story. For both these growth markets, we will continue to optimise our offerings for local demands to meet the country’s specific needs.
Overall, I believe that the pandemic has accelerated the speed of digitalisation. The COVID-19 pandemic reminds us that healthcare is part of a country's critical infrastructure. Expenditure for healthcare will come to be viewed as an investment in a country’s prosperity and competitiveness, and no longer as an annoying and unproductive cost factor. Consequently, development of the healthcare system will become a central issue on the long-term agenda for each country’s growth, along with ensuring ecological sustainability and expanding the digital infrastructure.
Every hour, around 240,000 patients are either diagnosed or treated on systems we have built, supporting our customers in the delivery of healthcare. We play a crucial role in fighting the disease. This includes the development and CE certification of a molecular test kit to detect a SARS-CoV-2 infection in record time, the fivefold increase in production capacity of blood gas analysers in just a few weeks, and the development of an antibody test with an outstanding sensitivity of 100 percent (14 days post PCR) and specificity of >99.8 percent11. We have put CT scanners in containers to help increase the supply in emergency hospitals and have developed AI algorithms to diagnose the disease. Beyond this, our role is to further enable the exchange and collaboration across nations. During the pandemic, we have provided a platform to share the lessons learned and actionable insights on how to tackle the COVID-19 challenge. As a global company operating in 70 different countries, we can help by connecting key stakeholders.
For our company, this means we will become even more important and relevant in the future. More than ever before, our customers and, beyond that, society and politics expect us to provide technical solutions to meet the enormous challenges we face. For example, these include solutions to digitalize healthcare systems, to improve the quality and efficiency of care, or to improve access to modern healthcare. As a company providing solutions for in-vivo and in-vitro diagnostics as well as in image-guided interventions and digital solutions, our goal is to enable healthcare providers across the world. I am glad to be in an industry where we can make a significant difference to people’s lives. It is up to us to play a decisive role in shaping the future of healthcare.
References:
1. Deloitte. (2018). What can health systems do to encourage physicians to embrace virtual care? New York.
2. The Economist Intelligence Unit. (2017). Global Access to Healthcare: Building sutainable health systems. London.
3. The World Bank. (2019). Current health expenditure per capita (current US$). Retrieved May 21, 2020, from World Bank website: https://www.google.com/search?client=safari&rls=en&q=Current+health+expenditure+per+capita+(current+US$)&ie=UTF-8&oe=UTF-8
4. World Health Organisation (WHO). (2008). Health in Asia and the Pacific. New Delhi
5. Caplan, L. (2014). Delay in breast cancer: implications for stage at diagnosis and survival. Front Public Health, 2(87).
6. World Health Organisation (WHO). (2014). A universal truth: No Health Without A Workforce. Geneva
7. eit Health, McKinsey & Company. (2020). Transforming healthcare with AI.
8. PwC. (2020). Mobile payments in Vietnam fastest growing globally, Thailand emerges second in Southeast Asia. Retrieved May 25, 2020, from PwC website: https://
www.pwc.com/th/en/press-room/press-release/2019/pressrelease-30-04-19-en.html
9. Ping An Good Doctor. (2020). Ping An Good Doctor’s Revenue for 2019 Amounted to RMB5.065 Billion, with its Losses Continuously Narrowed and Online Medical Services Revenue Doubling by 109% over the Same Period. Retrieved May 21, 2020, from Cision PR Newswire website: https://www.prnewswire.com/news-releases/ping-an-good-doctors-revenue-for-2019-amounted-tormb5-065-billion-with-its-losses-continuously-narrowedand-online-medical-services-revenue-doubling-by-109-over-the-same-period-301002912.html
10. Ping An Good Doctor LinkedIn Page. (2020). Retrieved May 21, 2020, from LinkedIn website: https://www.linkedin.com/company/ping-an-good-doctor/
11. Siemens Healthineers. (2020). Siemens Healthineers to expand SARS-CoV-2 testing to include a total antibody test to aid in the COVID-19 pandemic. Retrieved May 21, 2020, from Siemens Healthineers website: https://www.siemens-healthineers.com/press-room/press-releases/serologytest-covid-19.html