
Transforming healthcare will require a broad, interoperable Health IT system allowing healthcare providers to share and use patient data reliably and securely. This article outlines how US programs are supporting essential Health IT building blocks and how community Health IT partnerships can enable innovative programs for healthcare improvement.
As America embarks on improving healthcare, Health IT must be the bedrock for this transformation. While political debates rage over what a better healthcare system should look like, all proposed improvements will require a broad, interoperable Health IT system that allows healthcare providers to share patient data in a reliable and secure way and to use that information to improve the health of all.
Dr Donald Berwick (formerly of the Institute for Healthcare Improvement and U.S. Centers for Medicare and Medicaid Services) has summarised the goals of healthcare reform as the ‘Triple Aim.’ These three goals are better care for individuals, better health for populations, and reducing per capita healthcare costs. Health IT tools are critical building blocks for reaching these goals. Whether the initiative is to track quality and measure comparative effectiveness of treatments; share lab reports and images to avoid duplicate testing; mine public health data to discover and track diseases; expand managed care to new populations; implement standardised protocols to enhance safety and efficiency; employ home monitoring technology and telemedicine; or engage patients through portals, personal health records and employer-sponsored wellness programmes, Health IT tools are essential.
The basic Health IT essentials include:
Broad-scale adoption of Electronic Health Records (EHRs), with:
Creating this IT backbone for health reform will require an extended and concerted effort, the talents and expertise of many, and an investment of resources. This article will outline ways that US Health IT programmes are providing essential fuel for this journey and how partnerships across communities can build essential resources and enable innovative programmes for healthcare improvement.
Congress recognised the need for incentives and assistance to help hospitals and physicians adopt electronic health records when it enacted The Health Information Technology for Economic and Clinical Health (HITECH) Act, part of the 2009 American Recovery and Reinvestment Act (ARRA). This legislation, designed to promote adoption and meaningful use of health information technology, provided over US$20 billion in incentives through Medicare and Medicaid for hospitals and physicians who adopt ‘certified’ EHRs that meet national standards. Eligible physicians can receive up to US$44,000 each from Medicare or US$64,000 from Medicaid to help defray the costs of establishing a certified electronic health record system. To receive these funds, doctors must certify they have achieved
‘meaningful use’ of EHRs, including use of e-prescriptions and documenting certain quality measures and functions. The U.S. Department of Health and Human Services, Office of the National Coordination for Health IT (ONC), announced that as of June 2012, over 100,000 healthcare providers have received incentive dollars for adopting electronic health records, totaling more than US$5.7 billion.
The incentive program is helping spur change. In 2002, only 17.3 per cent of physicians across the United States had adopted electronic health records. In 2011, that number had increased to 56.9 per cent, with many more in process. In 2015, Medicare will begin reducing payments to doctors who have not implemented EHRs as a further incentive for adoption. Assistance in adopting electronic records comes from 62 federally funded Regional Extension Center (REC) programmes, which help eligible primary care providers acquire and use EHRs. The RECs provide hands-on, vendor-neutral assistance in selecting, implementing and achieving ‘meaningful use,’ of EHRs and enable providers to obtain Medicare or Medicaid incentive funds.
As of 2009, less than 20 per cent of physicians in the greater Central Florida area had adopted electronic health records. In 2010, the University of Central Florida (UCF) College of Medicine established a REC to help physicians in seven Central Florida counties adopt electronic health records and work towards the ‘Triple Aim’ of health reform. UCF has been awarded US$8.6 million through the American Recovery and Reinvestment Act funding to support the REC.
The initial local goal was to assist 1363 primary care providers with adoption and ‘meaningful use’ of EHRs. As of June 2012, UCF has signed on over 1300 primary care providers, and over 750 have ‘gone live’ on certified electronic systems. REC staff members help physicians and their practices achieve more efficient workflows by integrating the new technology, assist with privacy and security best practices, and have become trusted advisors to these providers. A recent customer survey found that 92 per cent of the physicians in the programme rated the REC’s work as exceptional and also helpful in minimising disruption of the practice while implementing an electronic system. The UCF programme is now expanding its services to specialists and dentists. The ultimate success of REC programmes across the nation will be measured as adoption rates increase and patient care quality and safety are improved. But this is only the first building block: as healthcare providers complete implementation of electronic records, they are asking, “When can I join the Health Information Exchange?”
A Health Information Exchange (HIE) is a data hub or repository that enables the sharing of clinical data among a patient’s different healthcare providers, bringing more complete and accurate information to the treating clinician at the moment of care. In addition to hospital and physician data, HIEs can include labs, pharmacies, imaging, home healthcare agencies, long-term care providers, and even insurance companies and other payers. By bringing together a patient’s entire medical history, these exchanges are a critical tool in building continuity of care and eliminating duplication of tests, a primary concern among patients. Recent studies are beginning to document the cost savings of information sharing, such as in emergency departments, where duplicative testing and unnecessary hospitalisations can be prevented. HIEs are increasingly used inside large health systems, linking hospitals and physicians within that system. However, these health system exchanges generally do not integrate patient information from community providers outside their particular system. A network of community, state, national and international HIEs must be created to link hospital systems, community physicians, ancillary and post-acute providers, and ultimately health plans. A coordinated system of health information exchanges will save lives, time, and money and can provide community data resources.
HITECH funding was allocated to many states for establishing HIE’s, but no single model has yet emerged for HIE technology, functionality, governance, geography, or economic sustainability.
In Central Florida, two large competing health systems, Orlando Health and Florida Hospital, have partnered with each other and with other community stakeholders to build a non-profit health information exchange known as the Central Florida Regional Health Information Organization (RHIO).
The organisation is committed to “Building a Healthier Community Through Connectivity” and just completed a successful pilot project that collected over 27 million records on over 1 million distinct patients. The pilot is used in 14 Central Florida emergency departments run by the two hospital systems. With the patient’s consent, emergency physicians can immediately access the patient’s clinical records from the exchange, which may include information on allergies, lab results, or an entire diagnostic workup performed at a different health system. The HIE access is structured for physician convenience and carefully imbedded into the physicians’ workflow, resulting in high use rates (ranging from 62 per cent to 87 per cent of available records searched.)
In a recent evaluation, 72 per cent of participating physicians said that because of the Central Florida RHIO information exchange they are ordering fewer lab tests, and 85 per cent said they are ordering fewer imaging studies. A study will be designed to measure the cost savings.
The Central Florida RHIO is now working to onboard additional hospitals, physicians, and ‘safety net’ providers who care for low-income patients. Plans are underway to have physicians currently served by the UCF Regional Extension Center join the health information exchange, and discussions are beginning regarding expanding the exchange to involve insurers and other payers.
The organisation’s Board of Directors represents community stakeholders such as hospitals, physicians, consumers, managed care companies, employers, ancillary providers, community foundations, and the University of Central Florida. This partnership has successfully tackled most of the common impediments for a community health information exchange, including technology, governance, privacy and security, and trust among competing providers. It is now working toward implementing a sustainable revenue model.
The commitment to creating a healthier Central Florida and the economic value of a centralised regional health information exchange and data resource are driving strong community collaboration in Health IT. Ultimately this partnership will deliver better quality healthcare, improved population health for the region, greater efficiency, and opportunity for economic development.
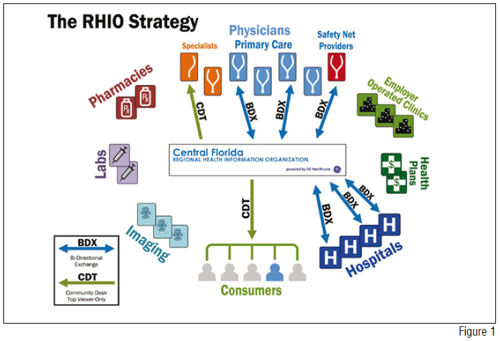
Figure 1 depicts the collaboration that is at the core of the Central Florida Regional Health Information Organisation’s vision
With electronic health records and health information exchanges in place, analytics and other data-use tools can be added to help monitor and manage diseases, improve services, coordinate care across communities, and in other ways help providers collaborate and achieve the ‘Triple Aim.’ This new technology is great medicine for a fractured, disjointed healthcare delivery system that is re-engineering payment incentives to reward positive outcomes, efficiency, value, managing chronic conditions, and staying healthy. For example, emerging uses of health information exchange can include programmes to identify gaps in care, demonstrate the most successful treatments, develop early intervention for at-risk populations, and improve care management (such as sending alerts to physicians when a patient is hospitalised or goes to the emergency department). Exchanges can enable use of data to identify threats to public health earlier and determine more successful solutions for high-risk conditions. In addition to improving quality of care, information shared through health information exchanges can help in identifying healthcare fraud and abuse, handling pre-admission hospital approvals and coordinating payments.
Some health information exchanges are also improving the way healthcare providers communicate with patients. They are developing portals so that patients and their families can access patient data, submit information and communicate consents. As a patient, imagine a single point for you to communicate with all of your healthcare providers, access your own health information and manage healthcare finances for yourself or your family member. Exchange portals can also tie in home- based technologies to support better management of chronic conditions like diabetes or high blood pressure day-to-day. With these types of portals, accessing your healthcare information could become as easy as banking.
The US government’s HITECH investment is driving Health IT adoption. Widespread adoption of electronic health records and a network of interacting health information exchanges can support emerging uses of technology and data, better communication and coordination among caregivers, better care for patients and more efficient delivery of services. Communities wishing to improve healthcare delivery and population health can collaborate to develop Health IT resources. Successful Health IT alliances can grow into broader community health partnerships, bringing together stakeholders, finances and human capital to improve healthcare for us all.

At the University of Central Florida College of Medicine in Orlando, medical students who grew up on computers and video games learn to practice medicine using simulation tools such as virtual patients that can be programmed to exhibit any symptom, behavior or diagnostic test result. These new doctors will demand the latest technology to support best medical practices in the 21st century. For that reason, M.D. students are issued iPads and computers and begin using electronic records from their first days in medical school, and the college is a national leader in the use of interactive, digital learning tools. UCF’s Health Sciences Library is 98 per cent digital, meaning faculty and students can get information in any location 24/7 on any electronic device. Most importantly, UCF medical students are selected for their humanistic desire to care for patients: they learn that technology is an essential tool, but that excellence in care for patients is the real goal.