The advent of 256 and 320-slice CT scanners will eliminate many of the technical difficulties that affect the temporal resolution of coronary CT angiogram. As technology advances, MDCT imaging of the coronary arteries will become the diagnostic tool of choice for the detection of coronary artery disease.
The main trigger for the onset of Acute Coronary Syndromes (ACS) following a prolonged period of coronary atherosclerosis is the rupture of an atherosclerotic coronary plaque followed by localised coronary thrombosis and / or spasm. The major factors that predispose to rupture of a vulnerable plaque are a relatively large lipid core, a thin cap, and an accumulated macrophage content. None of these determinants of plaque rupture are related to each other or to the severity of luminal stenosis.
Plaque rupture typically occurs at milder stenoses with 40 to 60 per cent diameter narrowing or less. These mild stenoses generally do not give rise to symptoms or ischemia on treadmill testing. The degree of stenosis in focal plaque segments on coronary angiograms does not correlate with the risk of plaque rupture. Plaques which have developed more recently are lipid laden, cause minor luminal narrowing and are more likely to rupture than older, hardened plaques with more severe luminal narrowing. It is therefore, not surprising that 65 per cent of stenoses associated with subsequent myocardial infarction have <50 per cent luminal diameter narrowing, and 85 per cent have <70 per cent diameter narrowing.
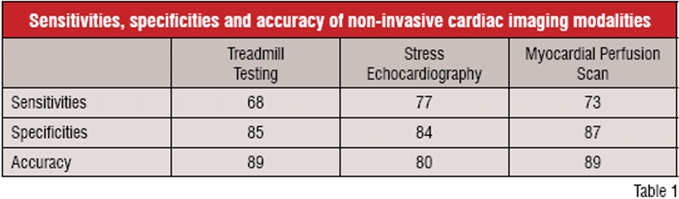
Conventionally, non-invasive methods for detection of coronary disease using stress treadmill testing, stress echocardiography and myocardial perfusion scan provide indirect means of diagnosing significant coronary disease where the coronary luminal diameter narrowing is more than 70 per cent. But they are unable to detect the vulnerable plaques that do not cause any significant functional stenoses, though they account for the large number of patients who eventually develop ACS. Coronary CT Angiography (CCTA) is one of the new modalities of coronary artery imaging. It is playing an important role in the assessment of coronary artery disease.
CCTA is performed by imaging the coronary arteries with a Multi-Detector CT scan (MDCT). Multiple sub-millimeter detector elements mounted on a gantry with a sub-second gantry rotation time, allow high-resolution axial images of the coronary arteries to be recorded while the patient holds his breath. A 16 channel MDCT scanner will have a lower volume coverage than a 64 channel MDCT scanner. Hence, the breath holding duration for a 16 MDCT CCTA is between 20 to 25 seconds, whereas for a 64 MDCT CCTA, it is 7 to 10 seconds. With newer 256 and 320-slice CT scanners which will become commercially available next year, the scanning time will be about 1 to 2 seconds.
With such a wide choice of non-invasive cardiac imaging modalities, it is important to assess each new modality on its own merits. Compared to current modalities, CCTA must be able to demonstrate accuracy of inferior quality for it to be used routinely.
Conventional non-invasive modalities for coronary artery assessment are performed to detect the likelihood of significant flow-limiting lesions but provide no information as to the presence of vulnerable plaques. They are also unable to detect the presence of sub-clinical atherosclerosis, which may predispose the patient to future cardiac events. Gender, cardiac rhythm, inability to exercise and the number of vessels involved may influence the results of these tests.
The sensitivities, specificities and accuracy of treadmill tests, stress echocardiography and myocardial perfusion scan are mentioned in Table 1.
Many centres, including our centre, have demonstrated that compared to invasive coronary angiography, CCTA has a high sensitivity and specificity for detection of coronary artery disease. At our centre, we were able to demonstrate a sensitivity of 99 per cent, specificity of 98 per cent, Positive Predictive Value (PPV) of 94 per cent and Negative Predictive Value (NPV) of 99 per cent for the detection of significant coronary artery stenoses. This compares very favourably with the other conventional modalities of non-invasive cardiac imaging. Hence, amongst the non-invasive tests, CCTA has the highest specificity and sensitivity for detection of coronary artery disease.
It is also consistent in most of the published papers that CCTA has a high NPV. The PPV of CCTA varies from centre to centre as different protocols and different post-processing methods are used. There is a tendency towards over-diagnosis initially, as there is a learning curve for CCTA. However, with proper patient preparation, experience, optimal protocols and appropriate post-processing techniques, a high PPV is achievable.
Increasingly, CCTA is being compared with Invasive Coronary Angiography (ICA). Unlike CCTA, which is able to provide a three-dimensional image of the coronary vessel including the vessel wall and the presence of plaque, ICA is a "lumenography" demonstrating only the lumen of the coronary artery without visualisation of the vessel wall or plaque. The presence of a plaque in a coronary artery segment is inferred from the narrowing of that segment relative to a wider adjacent segment. Hence, plaques which are not visible by ICA are visible by CCTA. A "normal" angiogram by ICA assessment may be abnormal on CCTA as some of the plaques may not cause an obvious reduction in the lumen size; this is usually seen in bifurcation plaques or diffuse plaques.
The limitation of ICA as a lumenography is particularly apparent in diffuse coronary artery disease. Intra-vascular ultrasound (IVUS) has been able to demonstrate the presence of diffuse, extensive coronary atherosclerosis in the absence of vessel stenoses on angiography. Compared to IVUS of the coronary arteries, the sensitivity of ICA to the diagnosis of diffuse coronary artery disease ranges from 7-43 per cent, with a specificity of 95 per cent.
In addition, the diagnostic errors in visually interpreted coronary arteriograms, where vessel diameter narrowing is visually estimated, are well documented. Even for cardiologists with extensive experience in coronary angiography, the severity of diameter narrowing is commonly overestimated by 30-60 per cent.
Hence, visual assessments of coronary angiograms severely underestimate mild or diffuse coronary artery disease and overestimate the severity of plaques which have >50 per cent diameter stenosis. Therefore, ICA as the "gold standard" for coronary artery disease has several limitations.
CCTA holds much potential as a highly accurate modality for assessment of coronary artery disease. Unlike ICA, which provides two-dimensional imaging and is essentially a lumenography, CCTA provides three-dimensional imaging and is able to visualise the coronary plaques and other cardiac structures. In addition, CCTA also has the advantages of being non-invasive, is less costly and is an outpatient procedure. In contrast to the known stroke and myocardial infarction risks of ICA, in the first 4000 CCTAs performed in our centre, there were no myocardial infarctions, no strokes and no mortality risks.
However, CCTA has certain interpretative pitfalls resulting from artifacts. The artifacts may be due to respiratory (poor breath holding) or cardiac motion (sinus tachycardia, irregular rhythm), beam hardening effects (caused by the presence of severe calcification, metallic stents, pacing wires), contrast related artifacts (produced by filling of adjacent chambers and coronary venous vessels) and post-processing artifacts (common cause of overestimation of luminal stenosis is due to "partial volume effect" during post-processing).
In experienced centres, using the 64-slice MDCT, CCTA may be comparable to ICA in sensitivity and specificity for the detection of significant coronary artery disease for the majority of patients. So it increasingly being used as the non-invasive tool of choice.
In the CARDIAC study (CT Angiogram as Replacement Diagnostic Investigation for Angioplasty of Coronary arteries-submitted for publication), a total of 121 consecutive patients in our centre, who were listed for PTCA solely based on the results of coronary CT angiogram were picked up for the study. We assessed the diagnostic accuracy of coronary CT angiography on a per patient basis. Peri-procedural complications such as Major Adverse Cardiac Events (MACE), stroke and emergency bypass graft surgery were evaluated. MACE including death from any cause, Q-wave myocardial infarction, and target vessel revascularisation during the next 30 days, were analysed. At the catherisation laboratory, following the pre-PTCA invasive diagnostic angiograms, 118 respondent (97.5 per cent) proceeded with coronary artery stenting. There were no periprocedural complications. Durng the 30 days, there was no episode of death from any of the causes: Q-wave myocardial infarction or target vessel revascularisation. Hence, in addition to providing an alternative to ICA, CCTA may allow better pre-planning of PTCA and hence, low complication rates.
The main risks associated with CCTA are the use of iodine-based contrast agents potential risks arising from radiation exposure during the scan.
Contrast risks are low. Post marketing surveillance of one particular contrast agent, Ultravist (data from Schering), showed that there were 14 serious adverse drug reactions in 75,000 patients (<0.02 per cent) Contrast risks are minimal and comparable for both CCTA and ICA for native coronary angiography. In the case of ICA of bypass grafts, the contrast load will be significantly higher as compared to CCTA of bypass grafts. With the 64 slice MDCT, Coronary CTA can be performed with as low as 50cc of iodinated contrast. The precautions to be taken for those with renal insufficiency are the same as in any examination, which require contrast agents. Most adverse contrast reactions present with rash and in rare cases, anaphylaxis can occur. From our centre's experience, for the first 4000 Coronary CTA examinations, we only had one case where adrenaline had to be given as a result of anaphylaxis. The patient did not go into shock and did not require hospitalisation.
The other main risk associated with CCTA is the radiation risk. In understanding the potential risks of radiation, it is important to understand the terminology. The term "radiation exposure," which quantifies the ionisation in the air produced by X-ray photons does not equate with the term "radiation dose", which quantifies the amount of radiation absorbed by the patient's body as a result of exposure to X-rays.
Radiation dose assessment is important for decisions on the risk-benefit value of the CT examination and to assess the effectiveness of measures for minimisation of radiation during CCTA. The fundamental radiation dose parameter in CT is the Computed Tomography Dose Index (CTDI), which is a measured parameter. The Effective Dose (ED) is the main parameter, which is used to compare the potential biological risk of X-ray examinations. It is commonly used to compare the different absorbed radiation dose and radiation risks of different X-ray examinations.
Unlike the CTDI, which is a measured parameter, the ED is derived from the CTDI. The SI unit for measurement of ED is the sievert (Sv) or millisievert (mSv). The ED is calculated from the relative weight radiation risks of each specific organ.
Reduction in radiation dose during CCTA has been made possible by two different methods. The first method utilises the fact that due to the elliptical axial section of the human body, the attenuation of the X-ray is less if the X-ray beam traverses in an anterior-posterior (AP) direction as compared to a lateral direction. Hence, less X-ray energy is required to produce a comparable image in an AP direction when compared to X-ray source in a lateral direction. The second method involves the optimisation of radiation exposure by ECG-controlled tube current modulation during periods of the cardiac cycle where cardiac motion artifact is minimised (ventricular diastole). Reduction of the tube current output in systole, when the likelihood of cardiac motion artifact is higher, can result in dose reductions of 45-48 per cent, depending on the patient's heart rate.
Many studies have been performed to study the radiation dose of CCTA. Some of the earlier studies had shown that the radiation dose from MDCT was approximately 4-7 mSv and was comparable to that from uncomplicated conventional coronary angiography. In a study where the ICA was performed by different cardiologists, the average dose varied from 3.1 mSv to 8.6 mSv. In a more recent study, continuous scanning with the newer 64-slice CT scanner without using ECG-controlled tube current modulation resulted in an ED of 13.4 mSv for males and 18.9 mSv for women. With dose modulation, the ED was reduced to 7.45 to 8 mSv for men and 10.25 to 11.3 mSv for women. This study assumed an effective mAs of 880. At our centre, when using the 64-slice CT scanner, the tube current for CCTA studies is routinely set between 500 to 600 mAs.
The increased radiation risk of CCTA is offset by the increased morbidity and mortality risks of ICA. In one prospective study, which investigated the risk of stroke embolisation following ICA, asymptomatic new cerebral infarction detected using MRI following left cardiac catheterisation occurred in 15 per cent of patients. Hence, invasive cardiac catheterisation carries a significant risk of embolic stroke--mainly "silent strokes".
ICA carries a non-radiogenic risk of mortality of 0.11 per cent, a major complication risk (excluding contrast reaction) of 1.3 per cent, radiogenic risk of mortality of 0.02 per cent and an overall mortality risk of 0.13 per cent (nearly two times that of CCTA) and major complication risk of 1.3 per cent. These risks do not include contrast reactions and silent strokes. In comparison, CCTA carries no non-radiogenic risk of mortality and no major complication risk. It carries a radiogenic risk of mortality of 0.07 per cent.
Hence, with proper optimisation of the protocols and settings, the radiation risk of CCTA can be minimised and the overall mortality and morbidity risks of CCTA as compared to ICA can be made favourably weighted towards CCTA. The main risk of CCTA is radiation risk. So protecting the patients from radiation is necessary. This means the justification for the radiological procedure is based on the premise that the potential benefit for the patient outweighs the potential risk of radiation. It also means that the ED for each procedure is calculated to assess the risk-benefit value of the CT examination and the effectiveness of the protocols and the settings in minimising radiation risks.
The development of the new CT scanners means that radiation doses will continue to decrease. Using prospective ECG gating protocols and new imaging sequences, radiation doses in 64-slices CCTA have been reduced to doses comparable to invasive coronary angiography.
CCTA can provide three dimensional view of the coronary vessel wall structure, heart muscle, valves, pericardium and even ventricular contractility function. It has a higher sensitivity and specificity for the detection of coronary artery disease compared with conventional non-invasive tests. Its main disadvantage is its potential radiation risk.
This is, however, balanced by it being the only non-invasive cardiac imaging modality with the ability to detect sub-clinical plaques, which may predispose to myocardial infarction and its ability to provide plaque characterisation. Hence, it can potentially play a role in risk stratification of patients with cardiovascular risk factors and provide physicians with added information on treatment decisions.
In contrast to ICA, which only visualises the lumen of coronary arteries, CCTA holds the potential for a comprehensive examination of the heart using one single examination technique. In addition, it can provide information on plaque distribution and characteristics which cannot be obtained on ICA. The examination is easily reproducible, objective and has a very high negative predictive value. In high-volume experienced centres, a high PPV is also attainable.
CCTA may potentially provide patients an alternative to ICA. In our centre, CCTA has replaced ICA as the diagnostic tool of choice for patients who are suspected to have coronary artery disease.
However, in some patients, the presence of severe calcification can present significant diagnostic challenges. The advent of 256 and 320 slices CT scanners will eliminate many of the technical difficulties that affect the temporal resolution of coronary CT angiogram.
As technology advances, MDCT imaging of the coronary arteries will be increasingly used and will grow in importance as a diagnostic tool for the management of coronary artery disease.