Care pathways are considered to be one of the best tools hospitals can use to manage the quality in healthcare concerning the standardisation of care processes, since they promote organised and efficient patient care based on evidence. It has been proven that their implementation reduces the variability in clinical practice and improves outcomes.
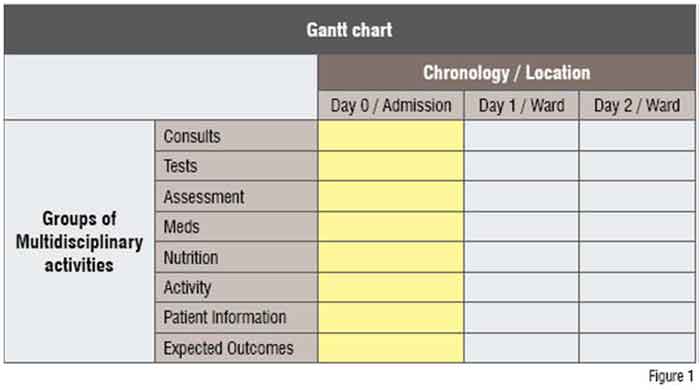
Care pathways are also known as Clinical or Critical pathways. A care pathway is a multidisciplinary healthcare management tool based on healthcare plans for a specific group of patients with a predictable clinical course, in which the different tasks or interventions by the professionals involved in the patient care (physicians, nurses, pharmacists, physical therapists, social workers etc.) are defined, optimised and sequenced either by hour (ED) or day (acute care). Outcomes are tied to specific interventions.
The care pathway concept appeared for the first time in 1985 inspired by Karen Zander and Kathleen Bower at the New England Medical Center in Boston (Massachusetts, USA). Care pathways are usually represented as a Gantt chart (Figure 1).
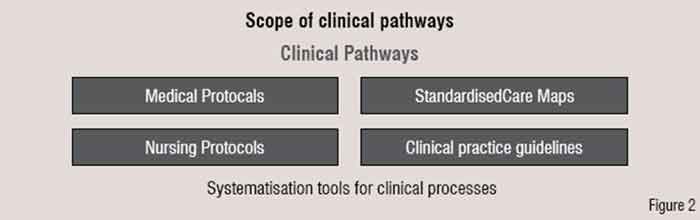
So far, different systematisation tools were being used for clinical processes. The oldest and most known are medical and nursing protocols. Over the last years other tools were introduced, such as clinical practice guidelines and standardised nursing care maps. Care pathways are care protocols that embrace all of these tools (Figure 2).
The main goal of care pathways is based on the improvement of the following areas: quality in healthcare, coordination / cooperation among professionals, efficiency and patient satisfaction. Thus, the purpose of pathways is the enhancement of care processes in three areas: quality, safety and efficiency.
Care pathways are a powerful tool for care process management, since they permit to check the compliance of all the interventions included in the healthcare plan, fix care standards and introduce clinical audits as a part of the process. Likewise, pathways are very useful to identify improvement areas in these standardised care processes,
under the umbrella of the culture of Continuous Quality Improvement (CQI).
The development and implementation of a care pathway involves a change in the organisational culture at any setting. This process may involve overcoming of some hurdles in its way of implementation. Following are some of the activities to be done to develop and implement a care pathway:
• Preparing multidisciplinary documents
• Reviewing the process by all the concerned staff
• Holding care pathway meetings to facilitate the exchange of opinions about patient care by different professionals
• Conducting periodic reviews to monitor some defined indicators
• Analysing variances or deviations
• Preparing common record documents for all the staff
Some barriers in developing and implementing a pathway are identified: the heterogeneity of patients and diagnosis, the common reluctance among organisations and professionals to change. These barriers must be considered by hospital managers since they may threaten a successful implementation of care pathways.
Methodology
The methodology of any project for care pathways implementation is divided in four phases: selection, development, implementation and evaluation. In this article all the steps will be comprehensively explained and some key points will be clarified in each one of these phases in order to help anyone who may be involved in such projects.
Selection
This is a phase in which the consensus is reached on care procedure to be followed in care pathway. Pathways should be designed for frequent and important (high risk / high cost) care procedures with an expected clinical course.
What should be the selection criteria? In order to standardise the process, following recommendations need to be considered:
• Multidisciplinary implementation
• Non-explained variability
• Outcomes far from standard
• Motivation by professionals to work on a specific condition
• Evidence-based Medicine, recommendations of good professional practices and professional references
• Possibility to reach a professional agreement at the hospital
At the start of the project, there are some tips to be kept in mind in order to build strong basis to prepare a good project. First of all, you need commitment and leadership from top managers (CEO, Medical and Nursing Managers) and a good communication from top to bottom This apart, project planning (please do not forget project management tools) and adequate resources (staff, time and material), which means a planned financial investment, are required for the success of the project. Concerning the hospital staff, you should transfer the ownership of care pathways to them and give them good training and education right from the beginning.
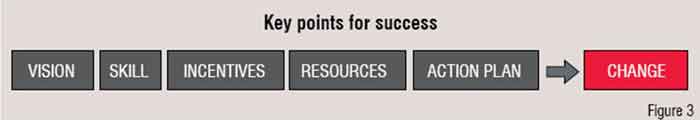
Above all, do not forget the economic incentives for staff to start a new organisational culture. When all the key points for success (vision, skill, incentives, resources and an action plan) are assured, one is very likely to get the key for changing the organisational culture (Figure 3). If not, this could result either in confusion, anxiety, frustration or a false start.
Development
This is the phase in which the care pathway is designed and the consensus is reached. The goals of this phase are the constitution of a multidisciplinary team as a ‘Care Pathway Committee’ (with motivation and ability of agreement) and the design of all the documents for a specific care pathway.
Requirements for developing a care pathway
1. Formation of the Care Pathway Committee by the Project Committee
2. Initial risk assessment by hospital managers
3. Examine the previous clinical audit of the process with retrospective data collected form medical histories
4. Evaluation of existing evidence and external practices (considering clinical practice guidelines)
5. Definition of the starting and ending point
6. Define objectives for each care pathway
7. Description of inclusion and exclusion criteria
8. Agenda of meetings with the Care Pathway Committee
The formation of the care pathway multidisciplinary teamwork (‘Care Pathway Committee’) is essential and the members should be very involved with the care pathway development. It is important to stress the need of consensus meetings. Professionals of the multidisciplinary team should reach agreements through the critical analysis of the different activities of the care process and the improvements to be introduced.
Implementation
This is the phase in which pathway is implemented. The procedures required for a right implementation are as follows:
1. Final approval to the pathway matrix and the rest of accompanying documentation by the multidisciplinary team
2. Approval by medical and nursing managers
3. Education and training for all the rest of professionals involved in the care pathway who did not participate in the Care Pathway Committee
4. Development of the ‘Implementation Plan’:
a. Decision of the start date for the care pathway new documents
b. Availability of the new record documentation
c. Appointment of a responsible person for each care pathway
d.New pre-implementation risk assessment
e. Internal communication
f. Training and education
5. Initial testing phase (usually two months is sufficient)
6. Review of the new documentation after this pilot phase
7. Official start of the care pathway implementation after this first review of the documentation
Although until now most care pathways at hospitals worldwide are managed on paper, the introduction of electronic pathways (‘ePathways’) at some hospitals has opened a new field for the improvement of care processes management. EIRA© is the software for care pathways management that is currently being used at two Spanish hospitals. Electronic pathways are the driving force to succeed in the implementation of care pathways.
And now let’s look at some lessons learnt during our projects for successfully implementing care pathways. The new record documents should be adapted to the existing ones in order to avoid too many changes for the staff, and always avoiding the duplication of any medical or nursing recording. In case of electronic Pathways, this specific software must be integrated with the common hospital information system.

Hospital top managers (CEO, medical and nursing managers) should ensure that each of these care pathways project is included in the hospital strategy planning and demonstrate their leadership from the beginning to the end. I always suggest them to attend the first care pathway committee meetings to show their personal commitment and interest in the project. At the same time, managers should promote the clinician management of care pathways to enhance the commitment of clinicians with pathways from the start.
Of course, there should be a hospital coordinator for managing all the care pathways implemented in the hospital. The coordinator should be a dedicated person having relevant experience of coordinating care pathways, and should posses leadership and communication skills. And he should be able to use a project management software (i.e. Microsoft Project), defining milestones and resources for each project phase. Together with the hospital managers, the care pathways coordinator must plan a strategy for communication, education and training.
A usual question is what to do with process management projects. Does process management interfere with care pathways projects? Must they start before or after care pathway projects? Process management means the upper dimension in the management of hospital processes. From my point-of-view, it’s more convenient to first define the core processes of the hospital with the respective process maps. If not, bottlenecks would be created when designing care pathways for concrete care processes and it could be already too late to solve them.
‘Evidence-based care pathways’ is the ambitious term used for any care pathway, but in fact you do not always find evidence for any procedure. Therefore we must search the best practice as a reference to design a care pathway.
In healthcare literature one can find some articles about how to measure the quality of a care pathway. One of the best tools recommended is the Integrated Care Pathway Assessment Tool (ICPAT). Developed by Claire Whittle (University of Birmingham, England, UK) and sponsored by the Strategic Health Authority of West Midlands (England, UK), it is a very practical questionnaire that allows you to evaluate the process of design, development, implementation and follow-up of care pathways.
A matter to be considered in the future is the involvement of patients in the process of designing care pathways. Since the main goal is enhancing their satisfaction during the care process, I think that we should face the patient needs together with the goals of the different professionals caring patients. The way to do it is an unknown factor, considering the problems sometimes to reach the consensus among the staff.
Evaluation / Follow-up
In this phase, the care pathway should be controlled, analysed and updated. Pathways are dynamic tools to be periodically reviewed and adapted, not documents to be left in the drawer.
In this last phase, the first activity should be the appointment of a responsible person for the care pathway follow-up. Who is suited for the job, a doctor or a nurse? Involvement of professionals from both medical and nursing fields are recommended in order to not discontinue the pathway compliance by all concerned physicians and nurses.
The next steps should be:
1. Establish dates for periodic reviews (recommended the first review after 6 months post-official implementation and then every 12 months)
2. A systematic and ongoing audit
3. Follow-up of the completion of the new record documentation (very useful in the first 12 months as a reminder for all the professionals)
4. Monitoring of variances with a fixed periodicity
5. Assessment and evaluation of the outcomes from the information recorded in the care pathway documentation
6. Analysis of the impact of the care pathway implementation on the care process
7. Feedback to managers and staff regarding the follow-up of indicators / outcomes and variances (essential to incentive staff to continue working on care pathways)
Updating the care pathway and documentation of its records is mandatory and should be done based on the publication of new scientific evidence, the information collected about the most frequent variances and considering the achieved objectives.
Regarding the analysis and evaluation of the care pathway, one of the most specific features of this methodology is the ‘variance report’—the information gathered from the analysis of the variance sheets. Variances (or deviations) may include activities that were carried out but not defined in the care pathway and activities defined in the care pathway but not carried out and medical complications. Different reasons may cause variances: patient and / or family, staff and organisation.
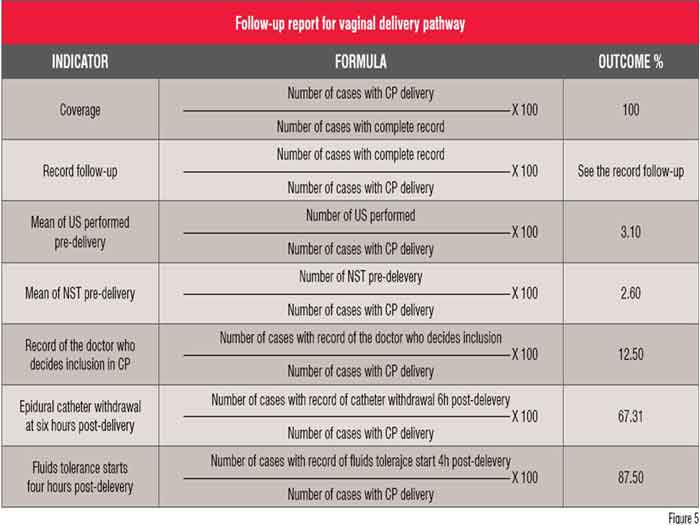
Another essential document for the evaluation of care pathways is the ‘follow-up report’, which includes the follow-up of the completion of the new record documentation, the variance report, as well as the assessment of the outcomes through the predefined indicators, which are related to the agreed objectives of the pathway. You can see an extract of a follow-up report from the vaginal delivery pathway in figure 5.
In conclusion, the methodology applied to care pathways projects is based on the continuous quality improvement (CQI), the P-D-C-A Cycle by Deming—Plan, Do, Check, Act. And start again.
Author Bio
Ricard Rosique is Senior Consultant at Diomedes and Head of Medical Department of B. Braun Group, Spain. He has contributed in developing methodology for the development of 120 Care Pathways (both surgical and medical pathways) in different Spanish hospitals. He shared his project experience at various conferences, seminars, congresses and courses in Spain, the UK, France and Portugal.