
The Covid-19 pandemic has made achievement of patient care in hospital systems an anachronism. Most hospital employees have lost interest and hope that improved excellence in patient care is achievable because of the general belief that top management lacks the skills to identify and constructively adapt to new medical challenges that require rapid response. Furthermore, healthcare workers feel neglected, poorly paid and often ignored when their ideas trickle up to those at the top. It is hellishly frustrating that middle management is even less qualified in the redesign and preparedness in focusing on processes and systems that drive employee motivation and patient care. The paper through the use of a case study suggests a practical approach to the implementation of Total Patient Care (TPC) in healthcare; a Systems Management approach..
The author is of the opinion that TQM is a process which embraces the conscious striving for zero defects in patient care and caring; the management of hospital organisations in co-operation with its workforce to improve processes in order to develop, produce and provide all medical services which satisfy patients’ needs and expectations. Although this represents a meaningful, detailed definition of TPC, Haigh and Morris (1994) contend that most managers find it impossible to work co-operatively with their employees to achieve improved organisational performance. This is because the structural adjustments are usually at odds with processes and patient outcomes as we have seen with lack of hospital capacity and mortality rate for Covid-19 patients. To achieve excellence, I am of the opinion that organisations must first map the business terrain by breaking down the organisation into three key elements: Figure 1.
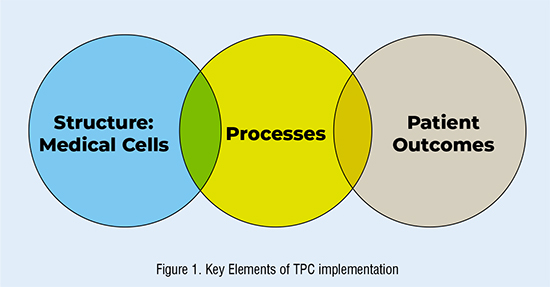
The author’s suggestion, therefore, is that quality patient care is fundamentally a structural decision determined at corporate level and must trickle down to all employees in cross-departmentally staffed medical cells. The structure must be focused on dedicated factories for dedicated medical care and resolution. Its success is dependent on middle management having a total buy-in and effectively implementing it with a proper thought out plan; with clearly defined quantifiable goals, roles and responsibilities for individual units, and having in place organisational norms that emphasise listening, supporting, coaching and rewarding staff appropriately. It should be noted, however, that at the initial stage of implementation, the success of TPC is not dependent on senior management commitment, but on a proper and effective implementation strategy championed by middle management, endorsed and made to work by a happy workforce, which would then have a domino-effect across the whole organisation.
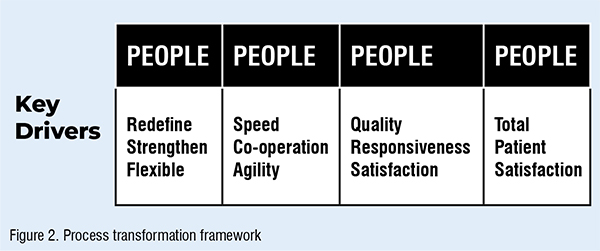
TPC is akin to playing basketball; it is simple, but we choose to make it complex by being overly technical. TPC is essentially a way of organising and involving the whole organisation; every department, every activity, every single person at every level focusing on the organisations’ core competencies in order to deliver continuous value to the patient. To that end, the authors suggest the use of a theoretical operations-based transformation framework at the onset of TQM as a guide for the identification of areas for improvement (Figure 2).
The sustainable transformation of an organisation to a TQM culture, in the authors’ opinion, requires a balance between organisational strategy, systems and structure (the way) with the fundamental commitment of staff, their skills, managerial style and values (the will): Figure 3.
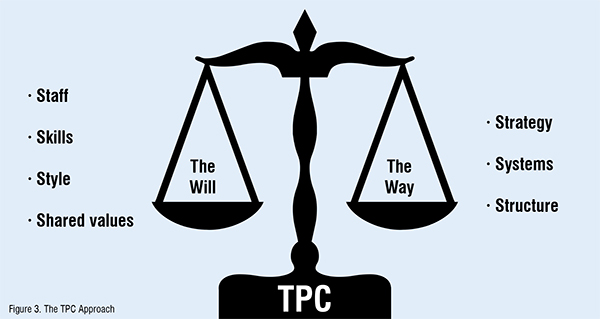
Without the development of the will, the ongoing success of the TPC programme would require a large amount of attention, effort, and energy to work against the fundamental status quo in an organisation, which dictates that ‘things should be done the way they have always been done’. The will can only be generated if TPC is accompanied by a plan to ensure that the behaviours encouraged are aligned with those required by the culture. Furthermore, as identified by the author the ‘WILL’ for ‘TPC’ must be fully developed by ensuring professional competencies are at the highest level and paying employees above market rate. The way is focused on servant and authentic leadership. Therefore for TPC to succeed, a ‘total’ re-orientation of employee beliefs and values is required. This is consistent with the views of Thomas Watson, Sr., the founder of IBM, who noted, “Any great corporation, one that has lasted over the years, will find it owes its resilience not to its form of organisation or administration, but to the power of values and beliefs and the appeal these values and beliefs have on its people (Arikian, 1991).
E-Healthcare came into existence on 1 August 2018. In total, E-Healthcare is responsible for an expenditure of US$560 million on health services, for its community. The main work of the E-Healthcare is to:
E-Healthcare employs a staff of about 2,200 across 5 hospitals, including part-time and seconded staff. The managerial structure of the organisation comprises of the chairman and five non-executive members of two statutory authorities and a jointly appointed chief executive. Their role is to oversee matters of policy and strategy, to monitor performance and ensure that the organisation operates to the highest standards of probity and accountability.
The organisation had to cope with the new changes that have been taking place to demonstrate an organisation wide approach to improving the quality of patient care through the development of quality improvement strategies which should be made explicit in business plans”.
Secondly, due to increased competition, the chief executive felt that the adoption of TPC would bring about a new cultural perspective that enhanced the need to provide medical services that meet the needs of the local community in terms of quality, speed, access, effectiveness, efficiency, comprehensiveness, safety, and appropriateness.
Furthermore, there were underlying barriers to be surmounted by recourse to the implementation of TPC within the organisation:
All of these factors had driven the management of E-healthcare to go down the TPC route. The organisation, therefore, through the adoption of total patient care, aims to ensure the provision of services which;
Structure
Process
Outcome
In the words of the patient care manager, the TPC programme was based on three major dimensions: Figure 4.
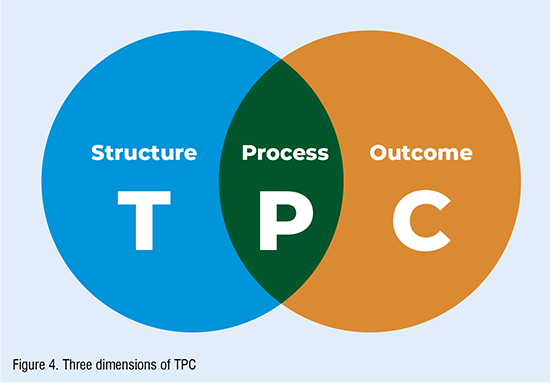
Quality, the manager suggests, “cannot be considered in isolation, as it is influenced by a range of factors: professional standards and aspirations, technical competence and skills, attitudes and social behaviour, consumer expectations and the resources available. Hence, all persons involved in the delivery of care, and the provision of support services, are key to the achievement of a high quality service”.
Stage 1:
The organisation had to first identify and adopt a clear vision based on what their main business and purpose is. According to the Patient Care Manager, the main purpose of the organisation is to “purchase the ‘best’ quality service for its patients”. The adoption of a vision based on the purchase of quality services provided clarity of purpose for all staff to work towards. In addition, a decision was taken by senior management not to introduce TPC as top management’s top-down rule, but as a home-grown approach where employees were allowed to voice their scepticism and make suggestions. Thus, employee involvement was seen as the first initial requirement of the TPC process.
Stage 2:
Involved the setting up of focus groups to identify gaps in service provision from the patient perspective. The focus group carried out a patient satisfaction survey across the county, which established a number of gaps:
On the basis of the patient survey, the organisation set out nine strategic priorities to deal with and close the gaps that were identified in the provision of services. The strategic intents included:
To cascade this definition across the organisation required a new organisational culture emphasising:
This new culture was to be sustained through an adherence to three core values: monitoring performance against agreed quality requirements between the organisation and its service providers; strengthening focus and developing patient empowerment developing quality medical cells and empowering staff.
The new system, according to the contracts/purchasing manager, enabled the organisation to deal with the initial barriers prior to TPC. To further ensure the internalisation of the three core values, the organisation made it mandatory for all its service providers to identify their corporate approach to quality and the responsibilities within their organisations for quality improvement, firmly linking these to their strategic objectives and translating them into key tasks and work programmes for each year. In addition, E-Healthcare asked a committee of employees to monitor progress during the year and evaluate clinical outcomes, which in turn informs the following year’s plans and programmes. To ensure compliance, the organisation introduced a uniform quality approach to be adopted (Figure 5).
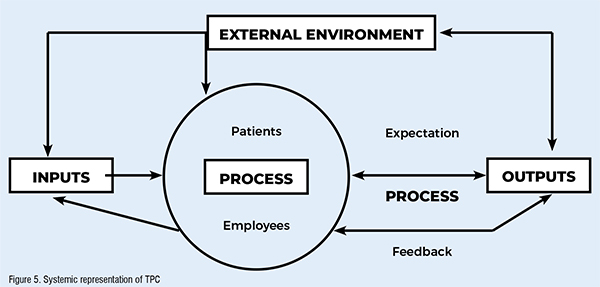
Using the above diagram as an illustration, what the case study seems to suggest is that for TPC to succeed, hospitals must work in partnership with its suppliers of service (inputs), involve patients and employees in the improvement and redesign of processes, in order to meet their expectations, which would result in the provision of a quality service (output). This requires the realignment of the entire organisational system to the principles of TPC, thereby creating a quality environment in which those with the primary responsibility for the treatment and caring of patients will work in concert. Any TPC implementation process that falls short of integrating and involving the ‘whole’ system would result in the partial implementation of TPC. A system is not the sum total of its parts, but the interaction of the whole.