As healthcare organisations focus their efforts to improving quality care and operational efficiency, accountability becomes a core component of their strategy for providing better clinical outcomes.
COVID-19 has pushed organisations across the globe into distress and healthcare organisations are no exception, due to increased demand for services amid mounting financial pressures. The pandemic has acted as a warning signal stressing on the importance of improving health surveillance systems and infrastructure, public health interventions. Emphasis lies on the need to develop preventive measures, improve technology integration, and increase remote care.
Virus outbreaks and COVID-19 pandemic have exposed the limitations, weaknesses and the lack of preparedness by governments and the life sciences and the healthcare industry. Hospitals and health systems have been unable to handle pressures resulting from the unprecedented increase in patient numbers. Despite public and private health systems focused on contingency plans, they found it tough to cope with rising demand. While critical to operate according to the need of the hour, it is important for hospitals—crippled with finances owing to halted out-patient consultations and limitation to perform critical surgeries—to maintain transparency in patient management. This will help build trust between patients and providers.
Implementing policies that lay emphasis on quality care through good governance and effective resource planning and management has become the key in the current scenario. Any discussion related to improving quality of care while reducing costs will tie back to accountability as the focus lies on maximising care, minimising medical errors, improving efficiency for better outcomes.
Accountability is in a way comparable to healthcare stewardship in the sense that focus lies on showcasing responsibility towards patients. Importantly, accountability in a healthcare set up results in providing effective care through efficient use of available resources that include human, technological, physical and financial.
So what encompasses the culture of accountability in a healthcare setting and why is it important to create a culture? It is essentially a set of policies and guidelines indicating evidence-based decision making and caregiving. Creating a culture of accountability is done by making learning and development a continuous process, increasing collaboration and coordination across all the organisational divisions, and leveraging performance management for outcome assessment and improvement guidance. Healthcare organisations can partner with the public administration to develop programs aimed at providing public health education to communities while also striving to understand factors affecting community health.
A major challenge with accountability of healthcare systems lies in lack of clear mandate on adherence to standard operating procedures. Another challenge facing hospitals and healthcare organisations is fraud. When left unaddressed, these can result in failure of quality care.
In the wake of pandemic, accountability and transparency have become criticalaspects owing to the risks of fraud. Fighting pandemics and global health emergencies may require regionalisation of capacities to improve community health. ‘Transparency’ contributes to making organisations accountable and these two are interlinked. Healthcare organisations are prone to fraud and corruption, specifically in the areas of contracting, facilities management, pharmaceuticals etc. Complying with standard operating procedures and guidelines, along with increasing transparency across all the activities enables mitigate the risk of fraud and corruption, thus facilitating provision of effective care. International organisations (IO) such as the World Health Organization (WHO), United Nations (UN) etc. have advocated the use of good governance as a key mechanism to reduce fraud and corruption in health systems. Establishing appropriate governance and accountability enables organisations to hold leaders and staff equally accountable for streamlined operations and effective care delivery.
Pandemics have occurred and may continue to occur, but our ability to overcome the challenges depends heavily on improving public health education, enhancing health systems’ capabilities to be effective and efficient in absorbing and serving sudden and heavy patient inflows. In today’s digital world, healthcare organisations can no longer cling onto legacy systems. It is important to deliver value to patients by integrating technology with clinician’s approach that translates into improved patient experience. Healthcare organisations ought to implement mechanisms that focus on innovative application of technology coupled with clinician engagement for continuous improvement of care delivery.
Another challenge facing healthcare organisations is the growing demand for quality care while reducing any untoward incidents and being transparent. This situation is not limited to a country or a region, but goes beyond political and geographic boundaries. When health emergencies and pandemics occur, we get to witness the deficiencies or irregularities in disease prevention and care giving to the global population at large.
When you create a culture of accountability, it facilitates growth and advancement of the organisation leading to sustenance in the long-run. It is important that there exists a sense of mutual responsibility that leads to increase in employee engagement, performance improvement and ultimately greater employee satisfaction. A key step towards making accountability an organisational culture requires leadership to act in a way to making it an integral part of the work. Leading with accountability is all about demonstrating that behaviour and thus helping professionals assume responsibility for their acts. This way, they lead by example communicating the need to be responsible for their acts and the entire organisation follows suit.
Another dimension is the use of performance management systems and quality initiatives to enhance quality and efficiency for better health outcomes. Has the approach helped healthcare organisations achieve desired results, as is witnessed in other industries? It can’t be a resounding yes because of the lack of holistic approach to changing the organisational culture that complements quality or process improvement efforts.
In order to bring about a cultural change, it is important to lay focus on breaking down silos, creating synergies and ensuring each and every member of the organisation is made responsible for his/her actions, while helping them with continuous improvement. By fostering the right skill development and empowering professionals, organisations promote high performance and create a culture of change. Shared governance coupled with accountability will lead to improvement at all levels beginning with individual departments, divisions and to the entire organisation.
Healthcare responsibility has predominantly revolved around the practice and approach to providing medical support and delivering care. This asserts the point that medico-legal issues cannot just focus on determining and evaluation of physicians’ negligence or malpractice. Historically accountability in healthcare was primarily assigned to doctors and slowly shifting to being shared by caregiver groups. Since healthcare teams deliver care, it is important to stop considering accountability from an individual perspective and making it a collective responsibility. In a collective accountability setting, individual health professionals have specific responsibilities in the broader framework of care delivery.
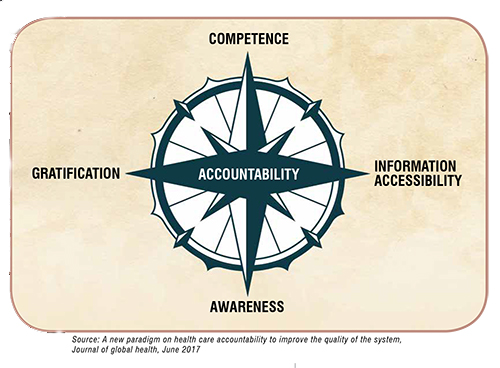
Each physician or doctor is expected to be transparent, play a key role in organisational initiatives aimed at evaluating medical errors and strategise plans for preventing those. Comparing different healthcare professionals’ approach in providing reliable support towards clinical risk management may offer some insight into addressing the issue from a treatment perspective. Accountability cannot just be limited to the impact of damage caused to a patient’s health. It should rather be made an integral part of the overall care giving from patient admission to discharge. What is required is a shift to improving professional accountability that can be based on four key parameters: competence, information accessibility, awareness and gratification. Developing competence and accessibility to relevant information equips healthcare leaders and staff in appropriate decision making.
Omar Ishrak, former CEO of Medtronic, had in the past spoken about how value-based care would be the future of healthcare and expressed concern that lack of accountability in healthcare could make it unaffordable to the population. Global healthcare community can take a cue from organisations that rely on value-based care in a bid to reduce costs without compromising on service quality. From a global healthcare landscape, effective health management can be achieved when health systems are committed to improving clinical effectiveness, lowering costs, sharing accountability, enhancing safety and, most importantly, making the population healthier. But striving to achieve these goals is a tough task in a complex and financially constrained environment that health systems operate today. Healthcare organisations will be able to build and sustain high performance healthcare culture by making accountability an integral part of care delivery.