
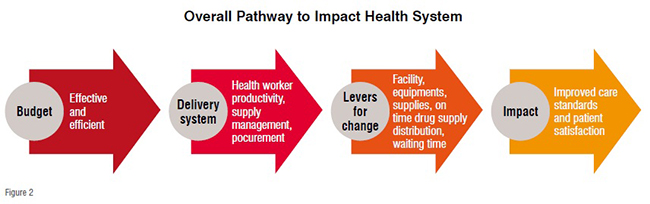
The growing demand for the quality healthcare and the absence of delivery mechanisms pose a great challenge, the key growth inhibitor includes fastest growing population and informal costs. Healthcare industry should be able to carry out planning, monitoring and controlling the delivery system in affordable cost. In response new service models, delivery plans, accountability between provider and citizens is essential for effective delivery system.
The growing demand for the quality healthcare and the absence of delivery mechanisms pose a great challenge, the key growth inhibitor includes fastest growing population and informal costs. Healthcare industry should be able to carry out planning, monitoring and controlling the delivery system in affordable cost. In response new service models, delivery plans, accountability between provider and citizens is essential for effective delivery system.

A healthcare system is the consortium of people, institutions and resources that deliver healthcare services; the sector involves hospitals, the pharmaceutical industry, the health insurance industry and medical technology industry. According to WHO, health services include all services dealing with the diagnosis and treatment of disease, or the promotion, maintenance and restoration of health. The challenge in the delivery of service depends on the way inputs are organised and managed to improve access, coverage and quality of the services to be provided to the users as well as providers. To have a well delivered health services management, leadership plays a crucial role along with good management for quality service delivery and advanced technology that will bridge the gap of accessibility and coverage of healthcare services to patients for reaching desired health outcomes.
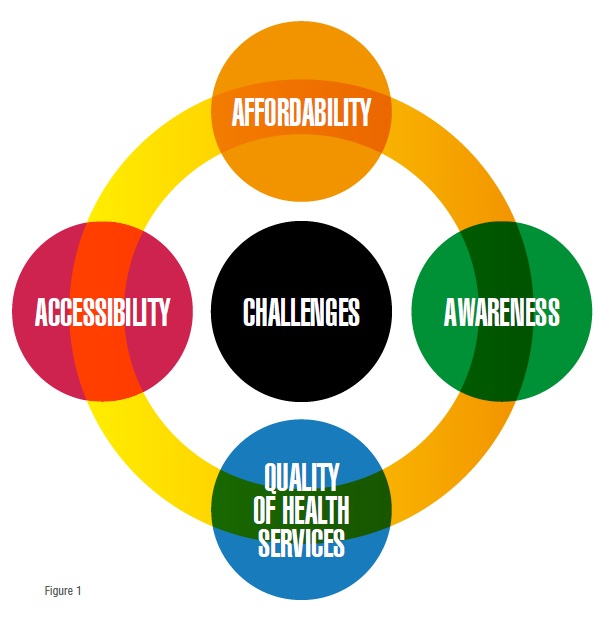
The challenges are faced at each level of system, starting from data management, treatment, patient follow up, providing services, payment, etc. Inadequate quality standard, unfavourable delays in passing the government bills and various reasons make our market commercially unfavourable for indigenous players. The challenges can be enlisted as,
• The rising population and awareness is leading to increase in demand of health services
• The rising informal cost of health services needs to be controlled
• Affordability of new technology by the common man should be ensured
• Focusing on providing quality service to ensure higher customer experience.
Medical insurance plans should be encouraged and out of pocket expenses should be reduced. New government policies should be up taken that will ensure less cost towards health services. Also, focus should be provided towards providing free medical services to patients suffering from diseases like tuberculosis, whereby a common man can afford and take benefits of health services. In case informal costs are enabled then the poor man doesn’t care about health leading to the transmission of the epidemics. Also policies and plans should be made for elderly age group so as to avoid informal costs.
New technologies like Electronic Health Records (EHRs) help in maintaining patient data securely and, whenever needed, the authorised person can view the details instantly like scanning the patient history, prior treatments, which acts as a reference that will help in diagnosis and prescription of medicines quickly. Telemedicine would help in bridging the gap between the patients and doctors across the world and provide better service from long distance. The quality of care can be measured looking based on hospital admission rates, patient feedback forms, length of stay, service provided to patients, hospital disbursements, equipment’s and technologies used, physicians visits, outpatient care and spending, home care service and cost, etc.
A clear dissimilarity in health status is observed between developed and developing countries, based on mortality rates, including infant mortality, young and child mortality and maternal mortality. With the help of organised plan and infrastructure, illnesses can be treated and deaths can be prevented. The account of expenditure spent on health services and quality provided should be accountable and effective management in delivery of health services should be provided.
The needs of rural population are quite different when compared to urban areas. The reason for this may be the difference in geographic, demographic, socioeconomic, workplace, and personal health factors. As we know the urban areas are polluted leading to breathing illness and lifestyle diseases are prominent among urban population. The rural populations mostly include baby boomers, GenX and children below the age 20, as most of the working population migrates to cities for employment.
The healthcare services are provided by public and private sector. Public sector in the healthcare industry is cost effective and affordable and provides services to urban as well as rural regions. The technologies used are not as advanced as in private sector but as per the need of the patients the government tries to cope up. The private sector is a well supplier of quality medical help, but is restricted to the urban populations’ areas and is expensive. Although the demand from rural areas is more they are more profit oriented and since there is no asurety about profit, these providers don’t see rural areas as a potential investment. The lack of economic investment leads doctors to work in foreign countries. There should be a way out and we need to standardise all our procedures and build clinics in the rural areas to improve efficiency. Another problem is lack of effective payment and insurance procedure.
Application of Telemedicine in rural areas: Two primary methods are involved in telemedicine: real-time telemedicine, and store & forward telemedicine. In real-time telemedicine the electronic telecommunication allows healthcare providers and patients to send and receive health-related information instantly. The most commonly used method for this is videoconference calls. This leads to rural population seeking more information from healthcare providers and significant reduction in waiting time period. In store & forward telemedicine, by means of emails, fax data is provided to the healthcare providers which they can access later as per their time availability. Due to long distance travel, many of the health services are unable to reach rural areas but telemedicine is one of the best ways to deal with it.
The process of healthcare delivery can be distributed in two parts: behaviour of professionals, and participation of people. Diagnosis of the illness including diagnostic procedure, diagnostic equipments, and treatment consists of recommendation of treatment, follow up to reassess the health. The participation of people includes promotion, advertising, utilisation of the health services, satisfaction with the provided services, and participation in decision making. In India majority of home healthcare services are delivered by community healthcare workers. The advantage in India is the services are more cost effective just the need is the workers should be effectively skilled.
Now-a-days the joint family system is vanishing, and job and other priorities are leading minimum care being provided to old people sick at home. A pathway can be designed to support people who have experienced a significant ‘event’ such as stroke, MI, or a fractured neck of femur, and illnesses which impact adversely on the person’s ability to live independently. Pathway can be designed focusing on delivering the time-limited interventions to those needful.
The National Association for Home care & Hospice says that 7.6million population is permanently disabled and chronically or terminally ill in the United States, and they receive home care services. The majority of population receiving home care services is over the age of 65, and they need support from someone to take care of them. As time is a limitation, family members are not able to pay enough attention and at such times home care services becomes useful.Also, it costs less compared to hospital stays, and provides access to a full range of services for people who need medical services throughout the recovery process.
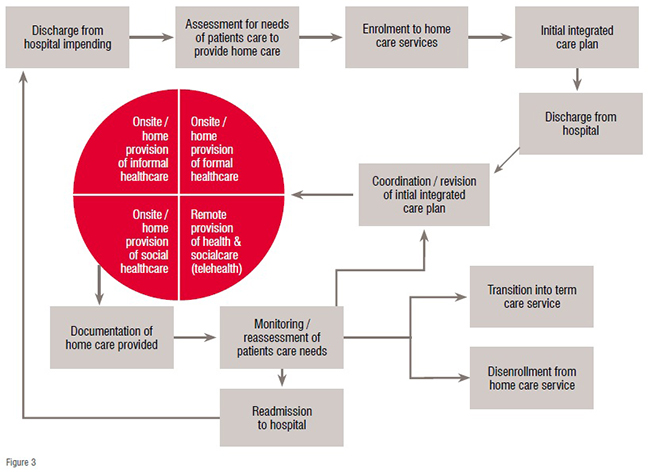
This can be divided into three stages. First is the entering stage, followed by receiving stage, and last, leaving stage. The entering stage may can be subscripted by service user themselves or a family member. The referral is followed by a needs assessment which targets both health and social care needs. The service user is enrolled into the services and an integrated care plan is designed, that includes a formal document that describes the services to be provided and the appropriate intervals. The receiving stage involves the personalised care delivery package combining informal, formal care; technologies like telehealth can be applied here. Documentation is a vital part of any process and has to be monitored for needs of patient care. If a case needs medical supervision, then the patient is readmitted to the hospital. The leaving stage involves discharge from the service or transition into term care service.
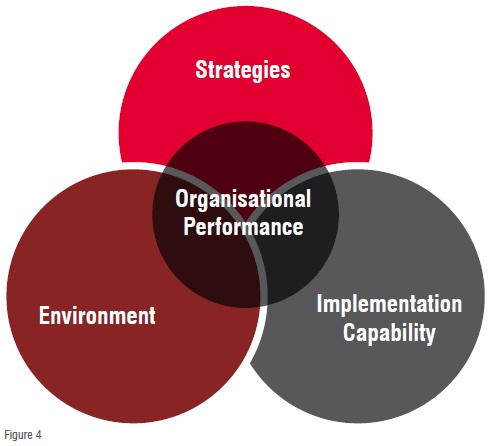
Hospital organisations and other health care firms have to deal with complex structures and situations in order to develop and impart strategies that will lead to positive change. The determinants of organisational performance consist of three variables: strategies, implementation capability, and environment. Before implementing strategies, it is important to know the root cause of the problem. Organisation can improve health outcomes by applying strategies at various levels, starting from own system management and at the level of individual health facilities. Reducing the waiting times of patient at health centres will save time of every individual involved in process. The following points can be applied for the same: (1) retraining and skilling the registration and medical records clerks, (2) relocating the cashiers, (3) adding up general practitioner, and (4) establishing a clinician for triaging the most severe cases to the emergency area and retaining the less severe cases in the outpatient department. Applying innovative strategies to improve service delivery such as new community-based organisations and workers, facility autonomy, results-based financing, and new information technologies will help in strengthening the healthcare system.
According to the WHO, health services are people centred and integrated, and are difficult to achieve. They support countries in implementing and developing policies, reforming strategies, designing and formulating guidelines. Patient centred services include diagnosis and treatment and other clinical aspects of healthcare services, whereas integrated health services involves management and delivery of safe and quality health services. Designing the pathways for various healthcare services by assessing the needs of healthcare providers and expectations of users, applying them in day-to-day life will make processes smooth and easy to follow. Integration of modern technologies like EHR, telemedicine in health services will save time, and provide excellent service to healthcare users.
References:
• https://ministerialleadership.harvard.edu/2016/05/finance-ministers-weigh-opportunities-and-challenges/
• https://www.slideshare.net/jamesmacroony/healthcare-delivery-system-in-india
• http://business.medicaldialogues.in/mtai-urges-govt-look-sub-categorization-devices/
• https://techstory.in/indian-healthcare-challenges/
• http://pilotsmartcare.eu/topics/integrated-ecare-pathways/the-smartcare-pathways/hospital-discharge
• http://www.who.int/healthsystems/topics/delivery/en/
• https://en.wikipedia.org/wiki/Rural_health#Application_of_Telemedicine_in_rural_areas