
It is the Culture not the Money. The competition to recruit, and the great advantage to permanently retain the best medical staff is not accomplished by money or flashy perks. It takes clarity of purpose, lived values, and real communication. The payoff is efficiency, quality and growth.
Engagement starts before the first day of work. The competition to recruit and the great advantage to permanently retain the best clinicians is not accomplished by money or flashy perks. It takes clarity of purpose, lived values, and real communication. The payoff is efficiency, quality and growth.
The shortage of high quality medical staff can be a crushing blow to a strong hospital or health system. Even in times of plentiful staffing, the highest functioning and most collegial providers may be in short supply. Your ability to compete, grow and serve the mission of improving the health and well-being of your communities will be impossible without a high-performing engaged medical staff.

There are many who are seduced into believing that it's all about the money. All I need to do is pay big and out - 'perks’ the competition and then you'll be in the driver seat. The data would imply that money is a week glue. Although you may be able to recruit some high performing staff members their ability to deeply engage in the broader responsibilities of the organisation will be limited if the only hook is their paycheck. Similarly , better benefits are attractive and can get people interested but studies show that not only are pay and benefits just a baseline consideration that ultimately will not keep great staff engaged, it also leaves you vulnerable to a bidding war with other like-minded big pay for your talent strategists.
Researchers would point out you do need adequate pay that is viewed as fair and responsive to both economic pressures and individual accomplishments. The benefits package has to be generally competitive and consistent with a long-term view of being part of a strong organisation. These are necessary but not sufficient.
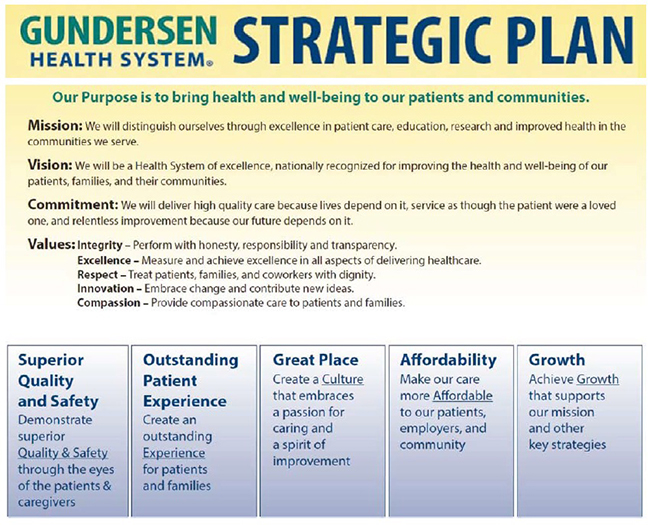
The pathway to much stronger recruiting and retention is not complicated it is just very hard It doesn't start in the interview room it starts in the boardroom. Clarity is needed from senior most levels of the organisation. What are the goals and priorities of the organisation? Why does the organisation exist? What is the long-term vision and plan? What will be the priorities for both short and long term? All these are important part of attracting individuals who are more likely to help lead your organisation to greater success.
If your goals are about crushing the local competition, or being 1 per cent better than you were before, or being a little bit better than your mediocre peers, it will not be inspirational for anyone. And it certainly will not be inspirational for the brightest, the best or the hardest working. These natural builders that you want to become interested and engage will look deeper at your organisation.
If your purpose is clear and the vision of how far you want to go in accomplishing that purpose is inspirational, the next piece to be consistent about is the environment they will be working in. Notice that we still haven't talked about how much money they're going to be paid, the call schedule, or the benefits. Of course these will be important and they all need to be discussed but if you're aiming for builders that will help lead the organisation forward, then we need people that are interested in what the values are and the likelihood that those values will be lived every day across the organisation.
You don't need a totally unique set of values. It is not the words… it is the consistency of action. They should be clear, understandable, defined, and most importantly, have a path forward to have them lived by everyone (especially the top most leaders)

Insightful candidates will figure out pretty quickly if your values say compassion but the staff don’t treat each other well so it’s unlikely they'll treat the patients well. If the value is respect and no one treats anyone with respect but it’s all rank based behaviour they will figure that out immediately. If integrity is one of the values listed , and the candidate is told to be careful about the contract because the front office can't be trusted, it is unlikely you'll be able to recruit or engage the best. The best performers have options they can go to; in order to really distinguish your organisation you need to be clear about your values and then live them consistently through recruitment, orientation, evaluations and every day practice.
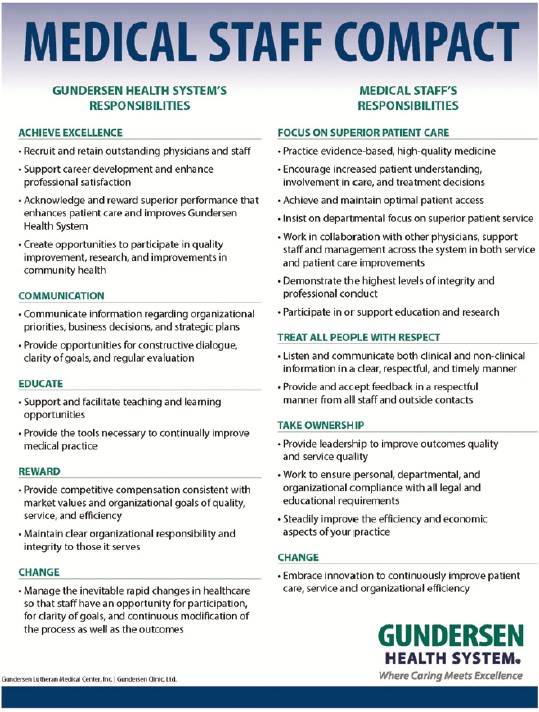
Many organisations have written this down so that it can be implemented, not just talked about. They developed a document called a physician or medical staff compact.
This is not a contract but it is a clear pathway for those looking to start their career or build their career. The organisation promises to deliver all those things on the left side and expects all of the medical staff to live those things on the right side of this document. This is a promise by the organisation and a clear request and expectation of the staff. It has been argued that these rules will limit interest and creative physicians might not come to an organisation or stay engaged.
That is not true. The highest performing, most creative physicians want to know where the guidelines for behaviour. They are interested not only in how they must behave but how they'll be treated, how their staff will be treated, how their families and patients will be treated.
So now you have built a pathway for physicians where the organisation sets high outward looking goals that serve a greater purpose, that aim for excellence, and internally, it is known how everyone is going to behave. Staff will be supported by the structure and clear promises from the organisation but they will also have an obligation to serve the mission and behave in a way that is healthy for all.
There is no intention to imply that it is easy to live these values or deliver consistently on the compact. You may have a high-energy member of the medical staff team who behaves very badly despite great quality outcomes, a tremendous work ethic and innovation well ahead of the curve. But they are so disruptive to other medical staff members and the support staff that there is a constant stream of complaints. Often senior leaders in healthcare have looked the other way and put a Band-Aid on the problem that needed major surgery. Short-term thinking would suggest we can just ignore this and move on, the clinician is too valuable to risk making them unhappy. But a longer-term and deeper look would show, and the data would support the fact that this type of behaviour affects the functioning of other medical staff members, the nursing staff and ultimately leads to dissatisfaction, retention and quality issues in an ever expanding circle. It is not complex…it is just very hard to keep that promise made by the organisation in the compact. It takes courage to be clear about your values and address them. It takes discipline to stick with your compact and your guidelines even when there are some compelling financial and even short-term patient care issues that may seem negatively affected. And finally you need durability. When you make these hard decisions for a long-term plan there are always short-term consequences that are going to result in you getting a great deal of push back. Building up that durability through consistency and connections with like minded leaders will be an important part of your work.
As important as these cultural buildings are, however, they are insufficient without several other factors.
Leaving communication to a chain of command is a very bad idea, it is an antiquated leadership style and has never been effective in business or healthcare. The chain of command is often the weakest link in a communication cascade. You need to strike a balance on what is the responsibility of the organisation and what is the responsibility of the staff member. What is expected of the organisation is clear communication in a timely fashion placed in multiple areas of access. The responsibility of the staff is to access the information online, in person, or written forms of communication that are offered. It is a dual responsibility. Of course, the medical staff is busy, of course they are burdened with many tasks and responsibilities, but they have to take part of the responsibility to avail themselves of the communication offered.
Along with responsibility to be clear comes the responsibility to manage change. The compact clearly states that you expect the medical staff member to engage in change management and be a leader in constant improvement. You lose the staff and their insight if the organisation doesn’t take seriously the responsibility to use those procedures and tools that will help them thrive and not be crushed as the pace of change increases. This is a huge distinguishing feature between great organisations and failing organisations. It will be a competitive advantage for those who can learn how to improve the efficiency of the staff again. Long-term, not short-term, thinking is what is needed. Short-term thinking would say ‘we don't want to take her out of clinic to learn these computer things, I am sure she will do fine learning along the way.’ You save a few dollars but end up with a frustrated, less efficient staff for months or years. Short-term thinking would say ‘no we don't want to add another medical assistant because of course that would add some costs’, but if adding one medical assistant increases the efficiency of the medical staff member by 30 per cent or 40 per cent then the cost differential is insignificant to the benefit in both quality and revenue.
When you look at studies about medical staff burn out and dissatisfaction with the job, they rarely lead with “I’d like my benefits 2 per cent richer”, they talk about the persistent struggle of change and support to help accomplish the levels of quality and efficiency they hope to meet.
One of our key responsibilities is to give staff tools to help manage this rapid change and the constant drive for improvement. Lean management systems have taken a lot of negative press with the weak comparison between building cars and fixing people. To the contrary, around the world, there is a growing number of high performing healthcare organisations proving you can engage staff, lower costs and improve quality at the same time. (Look at Catalysis https://createvalue.org/) Lean management practices can engage the front line all the way through the medical staff. They are simple to use and many of the tools are based on parallel principles that clinicians learned in medical school. For example, the A3 improvement tool can be used by anyone with any background but is engaging enough to have the medical staff quickly participate in improvement projects. The form asks you to describe the current state, very similar to a physical and history. It asks to collect data to support your position much like looking at lab and x-ray material. It asks you to describe the future state and reevaluate the changes you make on your way to that future state. It is very consistent with how clinicians, nurses and pharmacist train and makes for an easy transition to a staff building rather than staff crushing improvement projects.
Finally organisations that function very well invite the medical staff to be a part of the leadership. Engaging them rather than battling them results is better outcomes for all. The models may vary: physician CEOs or not, physicians highly represented on the board or not. The key is not who has what title. The key is to build a great environment for all staff, including the medical staff. If the medical leaders are willing to do that…then invite them in and the leadership team will be strengthened by their commitment and insight. The rest of the staff will be watching so the governance needs to demonstrate that the organisation is moving to serve the broader purpose, it's accomplishing it's major goals and that it's living by its values.
Several themes emerge from this description on how to build an environment that's more likely to recruit and retain your clinicians.
First a dual responsibility on the part of the organisation and on the clinician to agree to set broad goals focused on something bigger than themselves or their pocketbook.
Next, a set of values that are both clear, concise and consistently lived across everyone in the organisation.
A communication and improvement environment that is effective, efficient and improves (not burns) the life out of the staff member.
Finally , senior leaders chosen by their actions consistent with the purpose, goals and values and less so by their previous background or title.
The competition to recruit, and the great advantage of permanently retaining the best medical staff is not accomplished by money or flashy perks. It takes clarity of purpose, lived values, and real communication. The payoff is efficiency, quality and growth.
References:
1) Hariharan, S. (2014). Physician Recruitment and Retention: A Physician's Perspective. Physician Executive, 40(2), 44-48.
2) Steinbrook, R. (2009). Easing the shortage in adult primary care—is it all about money?. New England Journal of Medicine, 360(26), 2696-2699.
3) Holloway, E. L., & Kusy, M. E. (2010). Disruptive and toxic behaviors in healthcare: zero tolerance, the bottom line, and what to do about it. J Med Pract Manage, 25(6), 335-40.
4) Waldman, J. D., Kelly, F., Aurora, S., & Smith, H. L. (2004). The shocking cost of turnover in health care. Health care management review, 29(1), 2-7.