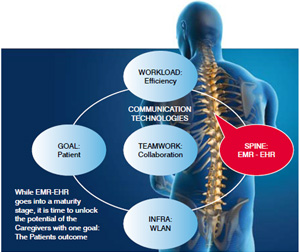
While the SPINE of the healthcare delivery-EMR-EHR-comes into a maturity stage, it is time to unlock its full potential by increasing the adaptation rate for caregivers via the implementation of communication technologies. Communication technologies linked to EMR-EHR can make it easier for caregivers to access EMR-EHR from any where, any-device. Collaborate between stakeholders, make workload automatically dispatched, while working towards one direction. The Patients outcome.
As the ‘spine’ of the healthcare delivery – the EMR - comes into a maturity stage, it is time to unlock its full potential by increasing the adaptation rate for caregivers via the implementation of communication technologies. The same communication technologies can be used to further increase the potential of the EMR by enabling the collaboration between stakeholders and by dispatching 'work tasks’ automatically to eliminate waiting times and increase efficiency. This will drive an improved patient outcome.
 While an outcome-based payment system is still far away, the implementation of an EMR system has already created a proven track of record. The EMR is now the ‘spine’. However, before it can function correctly it needs arms and legs and only then the knowledge (brain) can be developed and used to improve the outcome. We are all trained and passionate about helping patients, but the 'quality’ time per patient is decreasing fast, it is time to look into technologies that would help in delivering a patient outcome that is more predictable, less costly and has a better patient touch.
While an outcome-based payment system is still far away, the implementation of an EMR system has already created a proven track of record. The EMR is now the ‘spine’. However, before it can function correctly it needs arms and legs and only then the knowledge (brain) can be developed and used to improve the outcome. We are all trained and passionate about helping patients, but the 'quality’ time per patient is decreasing fast, it is time to look into technologies that would help in delivering a patient outcome that is more predictable, less costly and has a better patient touch.
The implementation of an EMR system is a time and money consuming process and already a huge challenge for the IT teams by itself. Linking all the clinical systems together and creating that single view per patient is easily said, but behind the scene each doctor, nurse will have their own requirements to make that single view work for her or him. A look at all the implementations around us, and we look a bit beyond the EMR implementation challenges, we see four new elements that are not directly linked to EMR but impacting the EMR adaptation rate, the healthcare efficiency, the collaboration between caregivers and how we close the loop by integrating the patient into this. Let’s look a bit closer to each of them:
Imagine that the IT team in an organisation comes out with the perfect EMR solution, including ‘that’ single view that each specialist, doctor or nurse has been dreaming about. But now put it into reality and as an example, we are following a doctor and head nurse doing their morning round in the ward. To be clear 'paperless’. In normal cases we will use the COW (computer on wheels). Let’s walk with them for one patient.
Clearly, nobody will use the system the way it is designed for and the nurse and/or doctor will write it down and starts adding things into the EMR when behind her / his desk with all the risks involved. So to make it practical, each caregiver must have access to ‘their’ EMR almost on a permanent basis. This opens the discussion to have medical tablets, like iPads, for each caregiver. Furthermore, doctors can use patient barcode scanning or even location tracking to make it easier to map patients with the correct EMR info.
So to me the first element to make EMR implementation a success and to increase drastically the adaptation rate is to implement a pervasive mobility concept that allows caregivers to connect all the time to their EMR views. What needs to be looked at to implement this?
The second element that needs to be looked at when using EMR is how it can help caregivers in reducing costs by optimising workflows. To make it clear, EMR is not per definition a workflow, or related to that, a workload management platform. What is known through EMR is all the major tasks that need to happen with each patient. Admission, tests (lab-radiology), medication and discharge.
Behind each major task you have a lot of small tasks that need to be executed in sequence by different teams. Let us take an example of a simple x-ray requirement
Specialist initiates a x-ray request into the EMR system
The above looks simple but try to add some real world complexity: what if there is a working shift change? Also, what is in most of the cases the reality? The specialist will ask the nurse to inform him when the results are available, more so when there is more than one task to be done like a lab test and an x-ray. So the nurse ends up checking the EMR for the results. There is a lot of room for workload optimisation.
Today there are a lot of point solutions available in the market to help a particular team in executing their tasks. A simple nurse call system is one of them. However, the more point solutions you add the more complicated it becomes. It is crucial to look into this with a very holistic view. None of the teams you have can work on an island; healthcare delivery is a multi-discipline, multi-team teamwork. So a workload management system should be as well and it should give you all the tools (intelligence) to make optimised decisions. Where are the bottlenecks? What is the expected gain if I modify this or add a person there? It is all about bringing the whole workload into a clear picture.
Next comes collaboration. EMR provides individuals (doctors) with snapshots of a patient. That is already a huge improvement over each doctor having some handwritten notes. However, we all need to recognise the fact that diseases become more complex and more and more patients will see multiple specialists simultaneously. How do specialists collaborate with each other? Are they not being trained as individuals in their specialty? Leaving that aside for a while, this is how the future will look like:
EMR is the only way to make sure that each care giver has a total picture of the patient, but it becomes even more critical that caregivers are able to discuss a patient’s situation on an ad-hoc basis. It is not that care givers would not talk to each other, as the goal of being a doctor is to help patient, but how can this be facilitated? In other words, how easy is it for a doctor to rope-in another doctor to discuss in two minutes the best course to help a patient. Let’s create a quick scenario:
 There is no need to go into more details, but as long we do not make it easy for a doctor to collaborate in an ad-hoc basis with colleagues it will not improve the situation. We are in a world where everybody is connected all the time with everybody. We have technologies like presence (knowing if somebody is available before you even dial his number), instant messaging, desktop sharing tools, video etc., yet these technologies are not linked into the EMR system, thus, not making it easy for doctors to collaborate. My last point is linked towards the patient centricity. Governments around the globe are all in consensus that we need to put the patient at the centre of the healthcare delivery as opposed to letting the patient come to the healthcare. In a world that is fast ageing and where people are able to spend more on their personal and family health, patient centricity is not just an option, it is the only way to go.
There is no need to go into more details, but as long we do not make it easy for a doctor to collaborate in an ad-hoc basis with colleagues it will not improve the situation. We are in a world where everybody is connected all the time with everybody. We have technologies like presence (knowing if somebody is available before you even dial his number), instant messaging, desktop sharing tools, video etc., yet these technologies are not linked into the EMR system, thus, not making it easy for doctors to collaborate. My last point is linked towards the patient centricity. Governments around the globe are all in consensus that we need to put the patient at the centre of the healthcare delivery as opposed to letting the patient come to the healthcare. In a world that is fast ageing and where people are able to spend more on their personal and family health, patient centricity is not just an option, it is the only way to go.
If all the above points of the EMR adaptation rate improvement via a pervasive mobile network are combined for improving the efficiency of the healthcare delivery and enhancing the collaboration between the caregivers, it would automatically contribute towards patient centricity. At the least, it would create a better dialogue by creating more quality time between the patient and the care givers. Healing people is more than a prescription of a medicine; in most cases it requires a change in habits or lifestyle and that requires much more talk time.
There is, however, one more simple point on patient centricity. In the EMR system it would be good if you could find all the scheduled appointments for a particular patient and even better if it would be possible to call-out or at least reach-out to the patient one day in advance of the scheduled appointment to double confirm that the patient will come. This exchange would allow the specialists not to overbook their appointments, and by doing so reduce the frustration of the patient.
If we leapfrog into the near future, say 3-5 years, patient centricity will be much more linked towards tele-health than today. If we are not able to solve the current issues or at least use the EMR system as the spine, we will never be able to move forward.
I hope that with these examples I was able to make some points clear. My only hope is that some of you out there are able to make the link between healthcare delivery and communications. What is described in this article is not a dream, it is full reality. However, it will take the hospital IT teams, the EMR providers and the communication providers some more time to make it a fully pre-integrated part. As healthcare is about teamwork, we all should put our hands together to make this happen.
Dirk has more than 20 years' experience in Europe and 9 years in APAC. His extensive expertise covers each domain of the business, from engineering to management, from infra to consultancy and he covers multiple industries like Government, Healthcare, Banking, Hospitality and Education. As a forerunner he launched successful Managed Services businesses, deployed service breaking City Networks and spearheaded the move towards industry specific solutions. He is a well know and appreciated guest speaker for various universities lectures and delivered key notes in major telecom events in Europe and APAC. Dirk is a graduate of Telecommunication and Microprocessors at the University of Antwerp.