
HCPs are most trusted sources of nutrition information and therefore, have a more critical role to play for their patients, especially in times of this pandemic. Beyond medication, HCPs can play a significant role in educating their patient’s about right nutrition and ways to leading a healthy lifestyle.
We have often heard of the adage, “A good physician treats the disease, the great physician treats the patient who has the disease.”The relationship patients have with their doctor involves a great amount of trust and vulnerability; and like any relationship, this too deepens with time. The encounters entailed in this relationship may not always be perfect and desirable, but it is one of the most moving and meaningful experiences shared by human beings.

Trust is a function of multiple aspects put together. According to the American National Institute of Health, trust, knowledge, regard, and loyalty are the four elements that form the doctor-patient relationship1, and the nature of this relationship has an impact on patient outcomes too. The quality of care, knowledge and time a physician invests in the patient is an important aspect. But what really drives the trust meter is a personal connection with the patient.
The pandemic has changed the world around us. Lives and functions of doctors and physicians are the most impacted. We are also entering the phase of AI and telemedicine that is enabling better access to consultation for patients who cannot transit in current situations. Conversational Artificial Intelligence2 (AI) for instance, is changing the way mental health care is delivered.
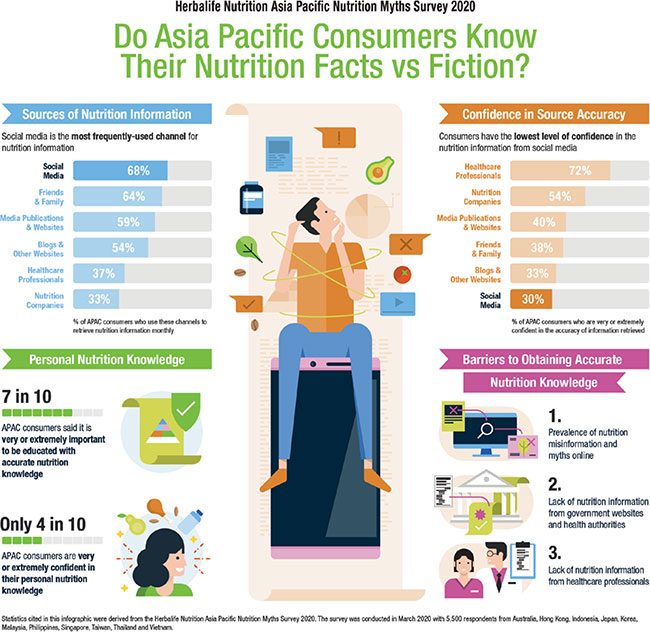
The current conditions require a new approach and opportunity for doctors. According to a surveyR1 conducted by Herbalife Nutrition in Asia-Pacific, it was revealed that the number one reason healthcare practitioners (HCPs) are unable to have an expansive consultation about general health and nutrition with their subjects is the lack of time. To achieve success beyond prescription, sufficient time for coaching and counsel is required. It often relates back to providing support in a patient’s well-being through counsel on diet, nutrition, exercise and lifestyle. One of the key insights derived from this study was that consumers (74 per cent) in Asia-Pacific were looking to HCPs as the most credible source of nutritional advice.
The physicians do have a new and more significant role to play in the new normal. As a continuum of trust and credibility healthcare providers are often playing the role of the healer archetypes, wearing the hat of health coaches. HCPs acting as a counsel, must adopt the “whole person” approach where, the patients are treated holistically3 – catering for their physical, mental and social needs. Attempting to better understand not only the patients’ sickness, but also their social, cultural and economic profiles and, above all, their expectations can greatly help the doctors in this new role.
Balanced and right nutrition is one of the key areas where healthcare practitioners can support their patients. The global rise of diet-related non-communicable diseases plus the double burden of obesity and malnutrition means that it is imperative more than ever that all HCPs are able to provide at least basic evidence-based nutrition advice.
A study4 on clinical level students from the University for Development Studies, School of Medicine and Health Sciences (UDS-SMHS), who had covered over 50 per cent of the curriculum noted that participating students believed that doctors should be the first ones to provide basic nutrition care and refer the patient to a nutritionist/dietician for specialised care if needed.
Improving an individual's diet requires more than just information, it requires consistent and long-term support to change and maintain new behaviours. While doctors acknowledge that nutrition plays a crucial role in health and agree that providing nutrition advice is part of their role, it is not a part of their regular practice5 sessions.
Time is one of the factors that is a critical enabler for imparting any form of advisory; in this case about nutrition. The current pandemic has resulted in more work hours and pressure for many doctors in the frontline and limited their ability to be available for such counsel.
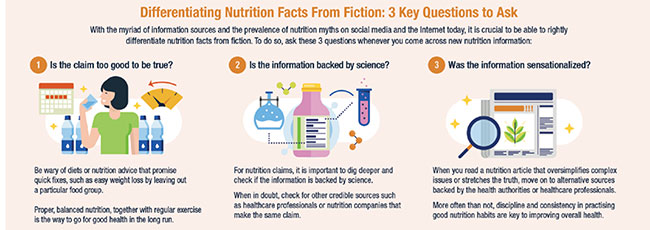
The surveyR1 conducted by Herbalife Nutrition in Asia-Pacific, witnessed a participation from HCPs and consumers alike. It was aimed at understanding the level of nutrition knowledge and information needs among these respondents. The outcomes of the survey indicated that 7 out of 10 consumers considered it extremely important to have accurate nutrition information and social media was the most frequently used channel in their search for answers. However, there are a cacophony of voices and opinions being paraded as nutrition facts and scientific findings, and consumer soften encounter information that are contradictory. The situation is exacerbated when there are unqualified individuals masquerading as experts. Suffice to say, cutting through the clutter to sieve out accurate and reliable nutrition facts is a challenge for many consumers who lack the basic tenets of nutrition knowledge.
Considering the high trust consumers and patients lay in HCPs,they have an opportunity to help patients shift to right sources for information, healthier food choices and share strategies to handle their food intake habits. Information about healthier fats, carbs, cutting sugars and overall better food and supplementation intake, active lifestyle, exercise and positive psychology should be incorporated in regular counseling sessions by the HCPs.

To know that your healthcare provider is there to support you in your journey, beyond prescription itself, creates a feeling of community and belonging for patients. As strengthening on this relationship becomes critical, so is the responsibility of HCPs to take on the role of providing adequate nutritional and well-being advice to their patients. Here are a few steps that can be taken to include nutrition advice in actual practice:
In parallel, health care practitioners should also take time to focus on their own wellbeing. We need them to be fully charged in this new normal. Taking care of their own physical, social, and mental wellbeing is critically important. There is a sense of fatigue that can occur and when we do not attend to our own need for nourishing our body and mind, we may burnout. As a healthcare provider, I want to encourage each practitioner to intentionally focus on nourishment for themselves as an essential worker that is needed by so many. Ironically, the patient-provider relationship can be a source of energy when it becomes an enriching experiencing focused on connection and support. Technology is an enabler that can be thoughtfully applied to maintain the human connection that both the patient and provider need. This level of support, beyond medication, may be a way forward that re-energises the HCP and provides hope for the patient.
References:
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4732308/#:~:text=The%2520doctor%252Dpatient%2520relationship%2520
has,fiduciary%2520relationship%2520in%2520which%252C%2520by
2. https://pubmed.ncbi.nlm.nih.gov/31681047/
3. https://apps.who.int/iris/bitstream/handle/10665/205942/B5022.pdf?sequence=1&isAllowed=y
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5809975/
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5809975/
R1. Herbalife Nutrition Myth Survey with 5,500 consumers and 250 healthcare providers in Asia-Pacific (2020)