To solve healthcare facility-related problems, planners need a new planning* paradigm and leadership, concerned with displacing old structures** with new; providing citizens with accessible, useful health information; achieving high patient satisfaction; and wrapping it up in an efficient physical environment that allows ease of wayfinding, is nonthreatening, and encourages personal control.
All one needs to do to observe inefficiency and patient dissatisfaction is to visit any healthcare institution that has not developed or adhered to a master plan for facilities, developed new facilities by focusing on individual profit centers, and thought more about technology and methods of billing than the patient and family experience of care. Unfortunately, these institutions are not hard to find.
Let's take a walk though one of these hospitals. What will we see?

'Telemedicine' typically refers to clinical applications of ICT, whereas 'Telehealth' reflects a broader application of ICT, including education, training, research and public health. The term such as 'eHealth' usually include the integration of electronic health records and health information exchange, and bio-medical informatics along with data analytics. South Korea uses the term 'uHealth' for ubiquitous aToo often a master plan document is developed in order to get phase one underway. Few institutions look beyond their initial financial budget to phase two, three, and beyond. In addition to efficiency, they need to consider how the institution is also responding to the public need, including urban design, parking, eventual full replacement, new models of care, 'wholesale' growth and internal 'organic' growth. Without a focus on the 'end game,' it's impossible to make wise investment sin facilities.
The advice we typically hear from strategic planners is that an institution should focus on one speciality, such as surgery, cardiology, orthopedics, women's health or neuroscience. This has merit in that these programs can be very profitable. However, few institutions are approaching the planning process with more synergistic planning concepts, such as an Interventional Department that consolidates many of these services or wayfinding systems that facilitate easy access or operational re-design to avoid transplanting old concepts of staffing and work-arounds to new a space.
The overarching cause of energy inefficiency is maintenance and utility costs related to buildings that have long out lived their ability to contribute to a 21st century model of care and technology.
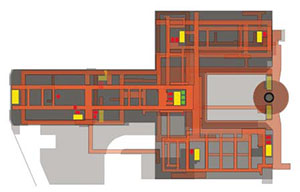
The reality of the low scores in patient satisfaction is two-fold. First the complexity and confusion related to navigation throughout healthcare campuses from garage to destination is all too obvious with most health centers. Over time these campuses have grown in ad-hoc ways, often expanding a department or adding space in the only un-built zone of the campus followed by running a corridor to this new location without thought of how a city planner might organise the streets of a new development. Imagine yourself as a patient under these conditions. This navigation process brings you to a crowded room with poor lighting, blaring TVs, no views and usually no daylight. If you can't distract yourself in a tattered magazine, you are left to simply look around at the other strangers in the room, none of whom are happy to be there. This waiting experience may be tolerable, but what is next is the experience of a treatment room that has only considered the machines and technology within, where you have no control, have lost any context of the natural world, and typically loved ones are only memories for the time being. Finally you are 'released' to try to find your way out because the wayfinding signs brought you there, but rarely do they tell you how to return.

Second, since the traditional design standards within the healthcare industry are so low, the drive to improve the environment for the 'client' or patient has no real business case strategy that most other service based industries strive toward. Therefore a patient may score a recent hospital experience based on a previous use of healthcare that could easily have been even worse.

What's really at the root of the problem? Simply stated, planners are stuck in an old paradigm.
What if these institutions developed leadership in new areas, say, a VP of Facility Organisation and Circulation? A VP of Energy? A VP of Patient Education? And a VP of Patient Satisfaction?
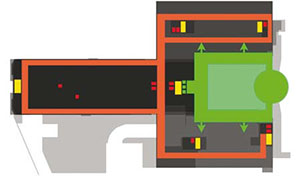
The VP of Facility Organisation and Circulation would be concerned about departmental adjacencies, wayfinding and walking distances. He or she would know that total GSF of a department is generally figured based on NSF of program spaces times a factor of 1.4 to 1.8 to allow for appropriate corridor circulation. This adds 40% to 80% of the constructed space. He or she also would know that widened corridors may be turned into program space, increasing the usable square footage of the facility.
Strategies that reduce corridors and improve organisation are directly related to 'lean' concepts of other industries and would facilitate patient observation, reduced hunting and gathering steps for staff, reduced areas of maintenance and contribute to patient and family access and wayfinding. This VP's contribution to the institution would add a new focus on efficiency, patient services, cross training of staff and facility optimisation.
The VP of Energy would know that older buildings are on average 28 per cent less energy efficient per square foot than new buildings. The question this VP might pose is not how an older building could be repaired one more time to extend its life but how is the institution strategically able to displace old space with new and how can those old dinosaurs be removed from the campus? This focus is not the traditional engineering department planning but one that looks at ROI not only based on facilities but how operations would benefit through the elimination of work-arounds, how care would increase in quality through better infection control, less slips and falls, more efficient tracking systems, reduction of lighting energy through harvesting daylight, research into grant funding for broad based energy savings concepts, etc.
The VP of Education may be the most proactive member of the leadership team. He or she would be more concerned about public health initiatives and ways to keep constituents out of the hospital. Population based studies would constantly tune the care team's expertise to the needs of the community. Educational initiatives would not only be the focus of patients and families but also up-steam initiatives, including community advocacy, schools, industries, new concepts in home health technologies and a broader reach in telemedicine distribution and utilisation.
Finally, the VP of Patient Satisfaction would assure good communications, outcome follow ups, patient accommodations, and possibly a more interdisciplinary service of care. The experience of visiting a hospital may be more akin to visiting the Apple Store. In both case you still wish you did not have to be there but the personal attention, anticipation of every need, expertise, elimination of a trial-and-error experience and a departing sense that your satisfaction was key to the institution would be more obvious
Again, all of this should be knit together with an efficient physical environment that allows ease of way finding, is non-threatening, and encourages personal control. It might be a very different hospital that emerges with this new set of VPs.
One can only imagine.
Unfortunately, the healthcare institutions that have not come to grips with the detailed understanding that significant change must be pursued are the institutions that will not be around in the future. Leadership in this effort must be bold and clear regarding the objectives. A leadership that sets a strong and clear agenda for change but then sways to the collective institutional politics will be short-lived, and the resulting facility plan and any coordination with future more efficient operations will become just one more book on the shelf.