
The electronic health record and its related technologies are new innovations that hold the promise of transforming healthcare. Nonetheless, all innovations encounter an uphill struggle of adoption. Meaningful Use and the HIMSS EMR Adoption Model are two complementary visions of how to make the promise of health IT a reality.
After receiving more than one thousand public comments to its Notice of Proposed Rule Making, the US Centers for Medicare and Medicaid Services (CMS) is crafting the final rule for Stage 2 of meaningful use of the Electronic Health Record (EHR).
While we wait for CMS’s final rule, it is worth considering EHR adoption in the USA and those forward-looking nations that served as early adopters of this transformative technology.
Innovation in any field is a challenge. Everett Rogers has studied the diffusion of innovations and explicated its mysteries.
Today it is common knowledge that scurvy is due to vitamin C deficiency and that a diet containing vitamin C will prevent scurvy. How we came to this understanding is a tale exemplary of the many twists and turns an innovation can make before it is finally adopted. The benefit of vitamin C containing foods like citrus in preventing and treating scurvy was discovered and re-discovered multiple times over hundreds of years.
Learning from the knowledge of the native people of the St. Lawrence River, the French explorer Jacques Cartier saved his men from scurvy in 1536. Decades later in 1601, Captain James Lancaster performed a controlled experiment in scurvy prevention. The Captain supplied one of his ships with rations of lemon juice and none to his 3 other ships. One hundred and ten (110) of 278 sailors died of scurvy in the control group.
More than a hundred years later in 1747, James Lind, a physician in the British Royal Navy, repeated the experiment with similar results. Ultimately in 1795 the British Navy did require citrus fruits to prevent scurvy.
Everett Rogers popularized this historical lesson and pioneered diffusion of innovations theory. Mr. Rogers would not be surprised by the history of the EHR, which is no less remarkable.
IBM partnered with Akron Children's Hospital to create the first electronic medical record in 1962.
Demand for this new innovation was nascent until the Institute of Medicine issued a trifecta of revelatory reports that defined the computer-based patient record as an essential technology for healthcare (later known as the EMR and now EHR).
Prior to the passage of the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009, physician and hospital adoption of the EHR in the USA was far behind Denmark, New Zealand, and Sweden. All three countries invested in economic incentives, regulations to foster interoperability, and public-private partnerships to enable standardization.
The HITECH act replicated many of these critical success factors with telling results. The rate of office-based physician adoption of a basic EHR system rose from 10.5 per cent in 2001 to 33.9 per cent in 2011. Hospitals with any EHR system increased from 15.1 per cent in 2010 to 26.6 per cent in 2011.
In the USA, the journey continues. Evidence suggests EHR adoption among physicians over age 55 and those in non-primary care specialties, physician-owned practices, and small practices trail behind that of younger physicians, primary care physicians, and providers in larger practices.
A digital divide has developed among hospitals, as well. Small, non-teaching, and rural hospitals have adopted EHRs more slowly than their larger, teaching, and urban counterparts.
The proposed Stage 2 goals build upon and expand those from Stage 1. Measures optional in Stage 1 will become required in Stage 2 (see Tables A to F). Taking another step towards capturing and reporting quality measures from the EHR, a host of new clinical quality measures will be added to Stage 2.
Citing Professor Rogers, the American Academy of Family Physicians cautions against raising the bar of Stage 2 meaningful use too high: “We encourage HHS not to ignore diffusion of technology theory, which distinguishes the characteristics and capabilities of innovators and early adopters from the larger grouping of early majority, late majority, and laggards. The existing data on Meaningful Use adoption, in our opinion, is limited to innovators and early adopters. Their ability and efficiency in use of electronic health records are not likely predictive of the ability and efficiency of EPs who have yet to embrace meaningful use. We strongly urge HHS to use caution in assuming that outstanding performance on Meaningful Use measures, so far, indicates generalised success and that the bar should be dramatically raised. Successfully on-boarding later adopters is likely to require a gentler approach.”
Indeed, the challenge for policy makers is striking the right balance between the vision of meaningful use with the everyday realities of limited resources.
Beyond regulatory relief, diffusion of innovations theory offers a framework to further the work of adoption. The theory posits four main elements in the diffusion process: (1) characteristics of the innovation itself (2) how the innovation is communicated to its target audience (‘channels’) (3) processes that affect the time to adoption (e.g. innovation-decision and innovativeness and adopter categories) and (4) the social system (e.g. system norms, opinion leaders, change agents).
The EHR itself can and should be made more usable and reliable. In a recent report on health IT the Institute of Medicine viewed this as a patient safety issue. User-centered design and reliable software also positively affect clinician adoption. The proposed new Office of the National Coordinator for Health IT (ONC) EHR certification rule takes a step in that direction by requiring user-centered design and software quality improvement. A better EHR will speed adoption, improve patient safety and clinician satisfaction.
The HITECH-funded Regional Extension Centers (REC) have been charged to provide a variety of adoption services for physician practices including e-newsletters, training, and on-site project planning and implementation. They are well-positioned to optimize services to promote adoption among small physician practices and small, non-teaching, and rural hospitals. Expanding and extending the RECs scope would help deepen adoption.
Meaningful use serves as one path for EHR adoption. Another complementary model is the Healthcare Information and Management Systems Electronic Medical Record Adoption Model (HIMSS EMRAM).
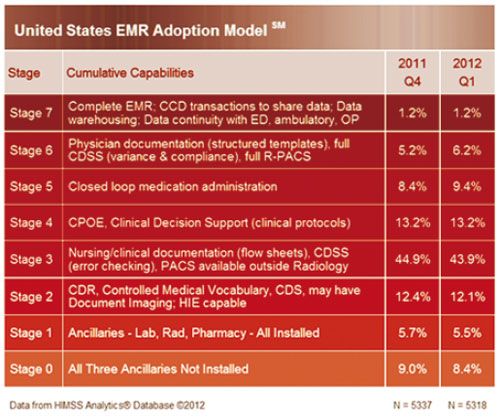
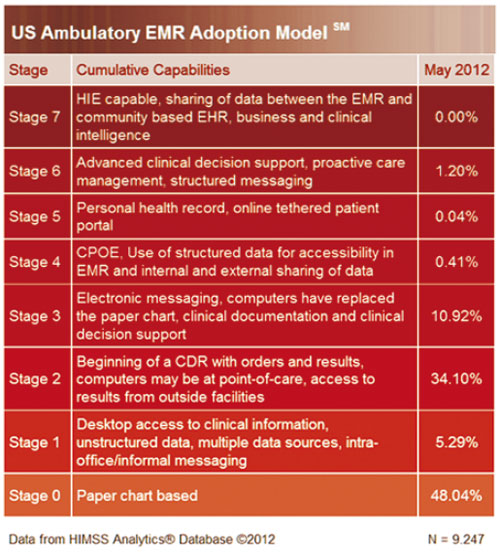
HIMSS developed the EMRAM for hospitals in 2004 and for ambulatory care in 2012 (see Tables G and H). The EMRAM serves as a tool for healthcare leaders to align IT initiatives with business strategy, develop a roadmap for future development, or ensure their organisations make the most appropriate use of funding. The HIMSS EMRAM permits healthcare providers and organisations to compare their IT budgets and level of adoption with their peers.
The HIMSS EMRAM has been used by hospitals in North America, Europe, and is expanding to the Asia-Pacific region. Launched June 2011, HIMSS Analytics® has collected data from hospitals from the Asia-Pacific (see Table I).
The Asia-Pacific’s first Level 7 hospital is Seoul National University Bundang Hospital (910 Beds) in South Korea. The area showcases another 13 hospitals that have achieved Stage 6.
It is all about transforming healthcare
Innovation is what drives health IT.
Meaningful use and HIMSS EMRAM are dynamic, not stagnant models for health IT adoption. Both models will evolve as new innovations develop to engage patients, coordinate care, improve individual and community health, and make healthcare more effective and efficient.
Stage 2 EP Core Objectives
Stage 2 EP Menu Objectives
EP CQM Measures: 125 Potential Measures covering the categories of conditions / disease management, drug management, preventive care and medical practice:
Stage 2 Hospital Core Objectives
Stage 2 Hospital Menu Objectives
EH / CAH CQM Measures: 49 possible measures covering the categories of conditions / disease management, drug management and medical practice
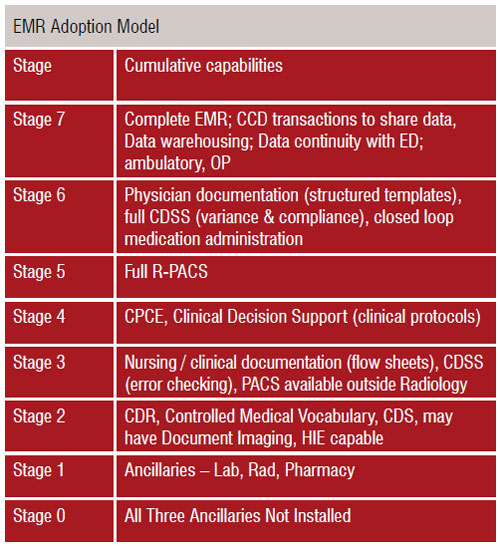
The HIMSS Analytics® Asia Pac EMR Adoption Model (EMRAM) was launched in June of 2011. HIMSS Analytics Asia Pac is focused on collecting EMR adoption data in the following countries