The YUHS planned a new EMR system that integrated pre-existing systems within the new system. The philosophical objective was to achieve first class medical services with safety, reliability and convenience through IT.
Every healthcare organisation always tries to deliver better services for its customers. Information Technology (IT) can be a representative tool for enhancement of healthcare services. The scope of IT can be a simple one to more complex one. However, in case of medical healthcare system any application of IT has to have the fundamental philosophy of “patient-oriented care”. To fulfill this philosophy, the application process of IT should be creative and innovative for individual health organisation. The best adaptation of IT to individual health organisation will guarantee the best ‘care processes’ for their patients.
According to the scope of IT application in the organisation, the objectives and process of development and implementation would vary.
Yonsei University Healthcare System (YUHS) is a healthcare organisation with four hospitals, three colleges and two graduate schools. YUHS has 2,500 beds and is the first westernised health organisation in Korea since 1880. Sixty four specialised medical departments are involved, and 600 clinicians and 8,000 employees are working in the main hospital. With respect to Hospital
Information System (HIS), YUHS has used several information systems in last 10 years, such as Order Communication System (OCS, same term with computerised patient order entry), Picture Archiving & Communication System (PACS), Human Resource System (HRS). The YUHS planned a new HIS that integrated pre-existing systems and newly-developed systems, such as Enterprise Resource Planning (ERP), Groupware (GW), Activity-Based Cost analysis (ABC), Clinical Data Repository (CDR), Disaster Recovery (DR) systems on basis of new system that included renovation OCS and EMR systems.
YUHS planned for an effective and ubiquitous HIS. The philosophical objective was to achieve first class medical services with safety, reliability and convenience through IT. To achieve this objective, YUHS planned the EHR system as a core system, which was beyond a simple order exchange system. Therefore, the master plan focussed on renovation of OCS, development of EMR system and then the integration of these two systems. The prime objective of the EMR system was the security of data and the privacy protection. On the basis of these objectives, the system has developed with the strategic consideration of standardisation, customisation, and authentication principles. The standardisation was done from code to the clinical document. The customisation focussed on user interface and special needs of end users. The authentication was done by adoption of new technology.
For many clinicians, EMR system, instead of paper recording, is regarded as a hard job to do, because there are too many patients for individual clinicians to take care and too many medical records to write in a limited time. This situation makes many clinicians hesitate to use the electronic recording system. They are afraid that they may not finish their work in proper time and may not have positive return on investment (ROI) consequently. Therefore, the development and implementation of EMR system in Korea meant more than the development of the system itself.
The EMR system had to be a realistic one that is fast enough to use, easy enough to learn, and also cost-effective. It also has to keep basic pre-requisites of EMR system, such as standardised terminology system and Clinical Document Architecture (CDA) that are necessary for future sharing of information and integrity of documents. This is not easy to realise. Therefore, many clinicians should give their knowledge and efforts, and all departments should change their working process under the new digital environment.
The acting groups were organised into several working groups (WGs). There were terminology WG, clinical document WG, User Interface (UI) WG, Authentication WG, Security WG, Nursing WG, CDR WG, Equipment interface WG, and CDR WG. All working groups comprised clinicians, nurses, paramedical personel and IT engineers. These WGs were focussed on their specific interest, such as standardisation of terminology, unification of data, maximum customisation of UI, job-defined authentication, nursing process, and security and private protection.
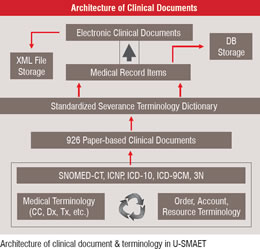
Figure 1 Process of Standardisation
The standardisation of terminology was accomplished by clinicians and nurses inside the organisation. Simultaneously, all codes of previous system were gathered from all the departments and unified between departments. This work of standardisation can provide the basis for a successful EHR system implimentation. Codes consist of codes of accounts, resource, medicine, laboratory, operation/treatment and departmental codes that are managed separately by each department. The standardisation of terminology was done by accumulation, analysis, classification, and new concept creation of terms. All record items with entered value were defined as Medical Record (MR) items and were gathered from the 926 paper-based clinical documents. As a result, MR items (15,092 items), Standardised Severance Terminology Dictionary (SSTD; 62,232 terms) and medical images (1,445 images) have been classified after a filtering and mapping process. On the basis of intra-organisational terminology, we develop the Clinical Document Generator (CDG) that can create XML formatted clinical document forms by simple selection of MR items (See Figure 1) This innovative process of clinical document generation makes possible convenient use and fast adaptation of the EMR system among clinicians.
After the establishment of SSTD and database of MR items, we mapped terms of SSTD and MR items with terms of the internationally accepted terminology system, to achieve future global sharing of information, such as, SNOMED-CT, ICD-10 ICD-9CM, ICNP, NINDA, NANDA, NOC. On the basis of above terminological architecture, all clinical document forms were created by CDG. The formation of document can be done by clinicians themselves and recorded. All recorded data is stored into the file server and database server for 22 months until now. ( Figure 1)
All clinical documents are stored in two ways. One is a storage of XML file with signature, and the other is a storage into the database of individual value of MR item. XML file storage maintains the interoperability and integrity of medical record, and database storage of MR item enables more efficient use of the information for the research and management of hospital. As next steps of implementation, we included the Disaster Recovery (DR) system into the basic architecture for the security of data at six months later, and built the Clinical Data Repository (CDR) at 22 months later for better clinical research and hospital management.
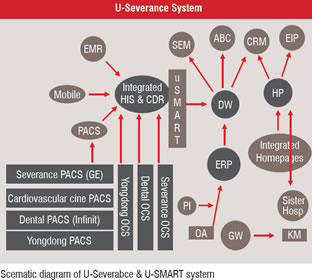
Figure 2 Development of Specialised Functions of EHR System
We decided to develop several specialised functions that reflect the organisation’s unique situation and culture, in order to enhance the safety and security of patient. They are as follows. Drug Adverse Effect Report System, Insurance Acceptance Guide System, Diagnosis Guide System, Antibiotics Dosage Control System, Child TPN Support System, Nursing Process System, Patient Information Control System, Specific Disease Marker System, Patient Education System, Double Check System with Barcode and RFID. These special functions were the results of active participation of clinicians and nurses in the project. Therefore, these functions can be the most ideal functions for the YUHS. After implementation, feedback from the users of these functions was obtained to improve and further develop functions to accommodate the users continuously. As for the authentication part, an ID-password system was developed. The smart card system with Public Key Identification (PKI) was adopted to verify the right individual for viewing and recording the data. This system is connected with the human resource system (HRS) of YUHS; therefore, change in job status can directly change the authority of medical recording. Finally, we named this core EHR system ‘µ-SMART’ (Severance Medical information Archiving & Retrieval System).
After 12 months of development, the Go-live plan was initiated and the final implementation was accomplished after 16 months of development. Go-live planning is crucial to the successful implementation of the system. The plan consisted programmes of education, simulation, and rehearsal with mock patients. The most important process was the education of end users. We planned three education programme; key user’s program, individual repetitive program and group program according to position, job and department.
The process of maximum customisation of UI is also important to the successful implementation. The customisation process of UI is a continuous interaction between final users and IT engineers. Post implementation, µ-SMART provides information to the other information systems, such as Enterprise Resource Planning (ERP), Activity Based Cost analysis (ABC), Groupware (GW), i-Severance (homepage), Parking system, Smart Card system (Figure 2). As a whole we have the system as ‘µ-Severance system’.
Getting the clinicians to participate was a tough task during the development. They don’t want to change their working process abruptly, and sometimes they cannot catch what they have to help or how they participate. Same as clinicians, there can be conflicts among paramedical departments due to their working boundaries. These situations can be aggravated because nobody can show the final result intuitively until the end of development. However, it can be safely said that the most important thing during the process was to continuously encourage of participation with passion. Any health organization has its unique culture and special working processes. As a result of participation, the individuals can know the strong and weak points of the organisation and their working processes. Only active participation can overcome any difficulties and can make the most effective EHR system. When everyone participates, it helps in learning more about the HIS itself as every participant can share his / her knowledge and have a strong interest for further development and better utilisation of the system. This kind of organisational upgrade was another result from the hard work put into the development of the EHR system.
Already 23 months have passed after the implementation. Now no clinicians and nurses can imagine working without µ-SMART system. Also we have found evidence of evolution, like the self standardisation of terminology, faster innovation of clinical document formation, better quality of recording, better working process and voluntary participation of new HIS projects. The economical effect and the Return on Investment (ROI) is still under investigation, however, we can be sure that there are many positive ROIs of EHR system. Further reports will be prepared in near future. We also have to keep the value innovation of EHR system to improve quality of care and to enhance the research capability, and also have to keep the technical innovation to integrate IT into the individualised home care of health.
In conclusion, I am sure that the EHR system improves clinical working process, patient’s safety and active utilisation of medical information. And it will realise ubiquitous environment of medical service in near future. The results of current EHR system will be another foundation for the sophisticated EHR system of the future, and knowledge-based medical services will become a reality. However, we should remember that people are always at the centre of the system.