Although providers see mHealth\'s promise to increase productivity in the healthcare system, they still exhibit reservations in moving quickly to adopt this new technology for several good reasons. Providers are looking for guidance in identifying, creating and adopting best practices in care delivery and are waiting to manage the broad array of challenges that this disruptive innovation creates.
Mobile health or mHealth has the potential to change the practice of medicine by increasing access and improving quality of care while decreasing costs. Yet lack of regulatory standards is limiting the rate and breadth of worldwide adoption. According to Emerging mHealth: Paths for growth, an mHealth study conducted by the Economist Intelligence Unit (EIU) and commissioned by PricewatehouseCoopers (PwC), 47 per cent of providers surveyed indicated that mHealth applications will not work with their organisation's IT, while 45 per cent of payers and providers said the lack of regulatory standards is stifling adoption. Based on these and similar findings, it would appear that standards in Information Technology (IT), care delivery, payment and regulation must evolve more rapidly for mHealth to realise its full potential as one of the most transformational movements in healthcare today.
In this article, PwC will provide additional insights about the mHealth marketplace and identify the standards required in six key areas that will enable the mHealth market to continue its upward trajectory of growth and success.
Healthcare systems, regardless of their level of economic, technical and clinical development face a common problem: they lack the necessary resources to deliver the same standard of care to those that require it in the future. Almost all regions globally face the following five constraints:
In developed countries, a rapidly ageing population is prompting the need for more healthcare services since 75 per cent of all healthcare costs occur in the last five years of life. In rapidly growing economies the problem is centred on the rise of chronic disease—often referred to as diseases of affluence—as standards of living for the population improve.
Shortages of healthcare professionals created by a combination of economic progress, ageing populations and retiring clinical professionals make it difficult to deliver care in the same manner as in the past. A recent survey of physicians in the USA indicated that one in three doctors plan to retire in the next 10 years. No country has the ability to produce enough healthcare professionals to close existing and future shortages without a radical change in the practice of medicine.
Shortage of hospital and institutional facilities, combined with budget constraints that limit the ability to build more means that care must be delivered in alternative locations such as the home, office, and distributed retail locations. Emerging countries, like China and India, with their very low hospital density ratios and rapidly growing and ageing populations, cannot keep up with the demand for hospital services to manage acute conditions. In developed markets, such as the USA or the UK, chronic diseases are usually treated and managed in existing hospitals, which represent 75 per cent of their spending.
With fewer resources to finance healthcare services, credit rating agencies have sounded the alarm that a failure to address future healthcare costs will result in downgrading a country’s credit rating. For example, according to the Organisation for Economic Co-operation and Development (OECD), Japan, which has the lowest spending on healthcare as a percentage of GDP among developed countries at 9.5 per cent in 2010, expects this figure to double in the next decade due to their ageing population. In the US, on the other hand, the figure in 2010 was already over 17.6 per cent and the US government expects it to reach 20 per cent by the end of the decade. These growth rates are viewed as potentially unsustainable and demand increasing levels of productivity to reduce them.
Command and control through top-down hierarchical structures will not solve the healthcare challenges. To deploy transformational change in a complex system among diverse, semi-independent and autonomous agents (doctors, hospitals, patients, etc.) requires a networked model of delivery as opposed to a hierarchical hospital-based system. IT fuels this complexity and requires us to rethink the structure and nature of a healthcare delivery system.
These five constraints make it clear that the status quo is unsustainable and productivity must increase, not incrementally but radically. Technological innovations, such as mHealth, have the ability to help overcome these challenges.
Mobile wireless technologies have already begun to transform other industries such as media, entertainment, music, publishing, banking, travel and retail. Consumers typically experience greater convenience, lower prices, more control and greater empowerment as a result of mobile adoption. Non-traditional companies have entered these non-healthcare markets with new innovations that have challenged the status quo and threatened the very survival of industry leaders. mHealth has the potential to do the same in healthcare.
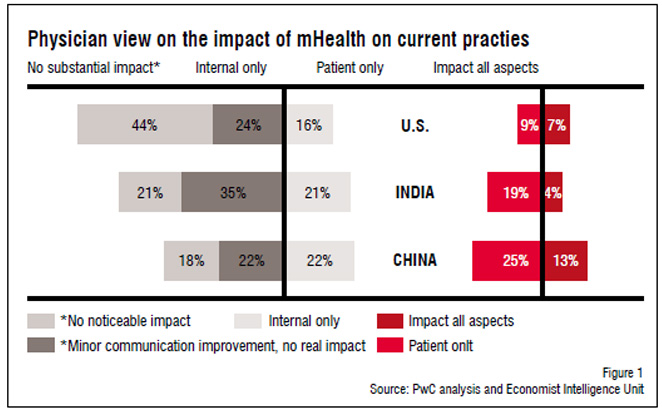
Yet while patients are receptive to mHealth, providers tend to be less enthusiastic, and opinions vary based on region of the world surveyed. In the EIU mHealth study, physicians and providers in China, India and the USA were asked what impact they expect mHealth would have on the current practice of medicine (see Figure 1). Among providers in these three markets, Chinese providers expected mHealth to have the most profound impact across the board, followed by India. What is interesting is that US providers think mHealth will be less transformative than providers in these emerging markets despite the ubiquity of mobile technology in the US among other industries and the US' dominance of mHealth applications and services over other markets. However, when these responses are viewed in light of the five constraints listed above, it's clear that they are more acute in emerging markets like China and India. Since necessity is the mother of innovation it is unsurprising that providers in those markets see such mHealth innovations more useful and essential to address their healthcare challenges than providers in the US.
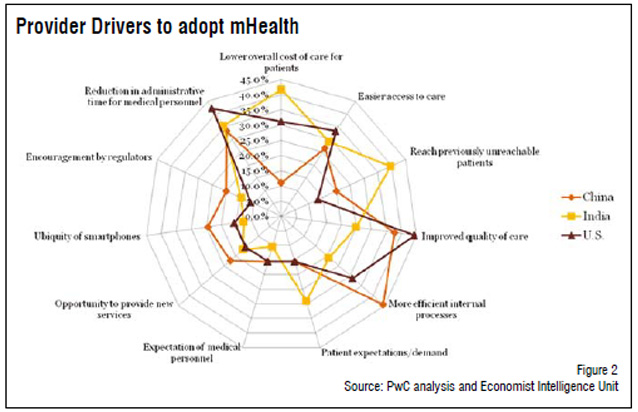
When trying to understand the difference in interest among providers and patients, we see that the key drivers for providers differ from consumers. According to the same EIU survey, patients across all three countries agreed on the four key drivers for patient adoption of mHealth: lower costs, greater convenience, better information and increased control over their own health. Yet among providers, the key drivers varied considerably across countries, as seen in Figure 2, and were primarily focused on the benefits mHealth can provide to the provider, not to the patient. This gap seems to exist between patient and provider largely because providers don’t view patients as a consumer. They, therefore, miss the opportunity to create new consumer-oriented value propositions by leveraging this new technology.
Although providers see mHealth's promise to increase productivity in the healthcare system, they still exhibit reservations in moving quickly to adopt this new technology for several good reasons. Providers are uncertain how to address the many new issues that arise from mHealth adoption and are looking for guidance in identifying, creating and adopting best practices in care delivery. In short, they want mHealth standards to manage the broad array of challenges that this disruptive innovation creates.
The following are some key guidelines and standards that providers should establish to allow mHealth to be appropriately leveraged to transform their practice.
Very rarely are physicians or nurses trained on how to deliver mobile care as a standard practice. For this reason, academic medical centres need to create an mHealth curriculum for existing students as well as alumni through Continuing Medical Education (CME) programmes. For example, the Veterans Health Administration (VHA) in the US had to create its own CME programmes to educate providers on these new care delivery technologies and practices. So far it has trained thousands of healthcare providers in its system.
To help subsidise this type of course, medical schools can partner with the private sector to enable real-life applications to be taught. For example, in the US, a global mobile technology company has helped fund the creation of an mHealth program at a Scripps Research Institute in La Jolla, California.
Clinicians are scientists. They demand research and empirical evidence that this new mHealth paradigm creates greater clinical and economic value than the existing one. To address this requirement, some organisations are documenting the necessary structures, practices and processes to quantify the economic value of telehealth and mHealth services. This research has then been used by others, such as the National Health Services in the UK, to develop their own programs.
Similar research, such as that published by the Mayo Clinic on e-visits, demonstrates that remote care can eliminate over 40 per cent of office visits without compromising the quality of care and substantially decreasing the associated costs. Similar studies, such as the hospital-at-home program recently published in the Annals of Internal Medicine show that moving patients into their home from the hospital can decrease costs by 30 per cent and improve the quality of life and care, with significant reductions in infections. As more research designs combine the dual outcome measures of cost and quality it will provide a standard for value that clinicians can use.
Healthcare is rapidly becoming an information industry, accelerated by the move to incorporate genomic information and patient generated data. Data and information growth in healthcare now exceeds that of all other industries, with volumes doubling every six to nine months. A key challenge, however, is that the focus on digitising existing medical records has left little time and resources to determine the best way to incorporate the data. As a result, much of this information, when generated and collected, is merely filed away with little thought to integrating it into other EMR or EHR records. This makes it very difficult for clinicians to use the information in a systematic way to diagnose, treat and manage patients.
In an effort to try and address this integration issue, some providers are aggregating the data through interoperable technologies and using intelligent algorithms to empower nurses and social workers who can do the type of work that was traditionally limited to physicians. This enables greater use of medical staff, increases staff capabilities, provides better patient care and decreases associated costs.
One of the greatest frustrations from those that have attempted to incorporate mHealth, remote patient monitoring, telecare, telehealth and telemedicine is that there is no ‘one size fits all’ standard for solutions. Factors such as disease, acuity, age, education, geography, culture and demographics all have an impact on treatment. Consequently, organisations that have attempted to create a templated, hierarchical and inflexible mHealth approach have been frustrated by failure.
The complex nature of healthcare requires the application of a simple solution based on several simple and common rules. An optimal approach tends to be consumer-centric, flexible, interoperable, and highly configurable and adopts the principles of personalised medicine.
Sony’s mobile division (formerly Sony Ericsson) in a presentation made at Capital Markets Day in Stockholm on 5 May, 2010, estimated that the number of sensors collecting data will explode from 6 billion to 50 billion over the next decade, with many of these being biosensors associated with human health. At the same time, the cost of these sensor and data aggregation technologies is dropping. Remote patient monitoring technologies that cost $5,000 just five years ago can now be had for less than $1,000, representing more than an 80 per cent reduction in costs. As the data collected from these sensors and mobile devices explodes, interoperability and integration as well as intelligent analytics will have to expand in order to use the information such that all the various components of any solution are ‘plug and play’
Various standard-setting organisations are critical to establish consistency for all the players in the healthcare system so they can deliver the best solutions for each problem. Some healthcare systems in countries such as Denmark and Japan have adopted interoperability standards to support a move to a more complex, adaptive system. More markets should do the same in healthcare just as they have done so in adopting telecommunication standards, to enable a thriving ecosystem.
Too often we have seen arguments that claim all we need for doctors to adopt mHealth is to pay them for it. While that helps, the fact is that the issues raised above generally pre-empt the payment discussion. If standards are not already in place to serve as a foundation then providers are uninterested in discussing reimbursement.
After studying various mobile technology business models from other industries, and the way and pace in which they have rolled out, some important lessons have emerged
While technology is a powerful enabler, it is only one element among a host of requirements. A number of standards must be in place before the case can be made that mHealth is a viable and sustainable solution in improving productivity and addressing many global healthcare challenges. A mutually supportive ecosystem of standards across all aspects of mHealth will enable a new paradigm of healthcare that addresses the acute needs in all countries for all people.