
With the size and costs of RFID tags decreasing, their incorporation in surgical sponges, endoscopic capsules and endotracheal tubes is creating potential benefits in patient safety and diagnostics.
In 2005, the Dutch Ministry of Health, Welfare and Sport initiated a project with RFID in healthcare. Capgemini, Geodan, Intel and Oracle implemented three applications at the Academic Medical Center (AMC) in Amsterdam. The applications were based on the use of active and passive RFID tags. The Geodan Movida platform managed all identification, location and other attribute information. Next to these applications the project created an overview of best practices and standardisation issues of RFID inside and outside Europe.
Applications that facilitate logistics and inventory management of expensive medical equipment appear particularly promising in the healthcare industry. And because the size and costs of RFID tags are decreasing; their small size permits incorporation in surgical sponges, endoscopic capsules and endotracheal tubes with potential benefits in patient safety and diagnostics.
Essentially, Radio Frequency Identification (RFID) systems collect information about physical objects automatically. Because information about tagged objects can be transmitted for multiple objects simultaneously through physical barriers and from a distance, RFID has an advantage compared to reading barcodes that require ‘line-of-sight’ and active user interaction to access the enclosed information. RFID systems exist of three main parts: (1) the tag, which is the identification device attached to the object being tracked, (2) the reader that recognises the presence of a tag and reads and processes the information which is stored on the tag and (3) the antenna, which is part of the communication between tag and reader.
Tags are also called transponders and basically exist of three types. First, passive tags do not have a battery and derive their power from the radio frequency signal broadcasted by the reader in order to be able to transmit their data. Second, active tags have a battery and a transmitter, and do not rely on the power derived from the reader to operate. Third, semi-active (or semi-passive) tags have a battery and use the radio frequency signal broadcasted by the antenna to be activated in order to communicate. Semi-active tags can also contain sensors (i.e. temperature or humidity) that can be used as data-loggers. The tag ‘wakes up’ at pre-defined times to update the data collected by the sensor. Activation by an antenna is not required.
RFID systems operate at frequencies ranging from low frequency (LF) at 125 kHz to microwave at 2.45 GHz. The latest one is also known as the technology used for Wireless Local Area Networks (WLAN). Lower frequencies are able to penetrate through materials, while better and higher frequencies can process more data. Based on these and other characteristics like the risk of electromagnetic interference or the object of interest, the most suitable RFID system can be applied. In order to track patients or medical equipment through your facility, an active or semi-active RFID system could be appropriate. For inventory control or blood product patient matching at the Operating Room (OR) a passive RFID system might be sufficient. In the pilot, a semi-active RFID tag with a temperature sensor was used for tracking blood products.
The application of RFID at the AMC in Amsterdam were conducted in a large-scale pilot that was carried out at the Operating Rooms, the Intensive Care Units (ICU) and Blood transfusion laboratory. The purpose of the pilots was to show the added value of RFID in Healthcare, with a special focus on patient logistics, patient safety and disposables efficiency. The goals of the first pilot were (1) to acquire insight into the patient’s journey through the OR-complex and (2) to understand movement in and out of the operating room. The second pilot addressed the issue of location and temperature monitoring of blood during the entire transportation and storage process. The third pilot focussed on the accurate measurement of the use of expensive disposables.
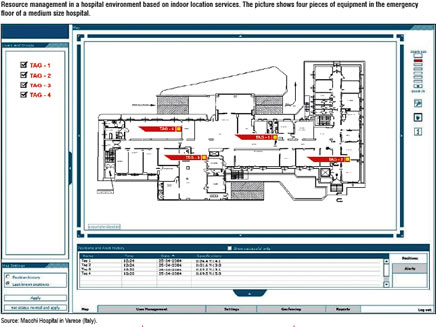
The central software system Geodan Movida, collected and processed data of the ID and location of patients, blood products and disposables. It also provides alerting capabilities, to prevent, for instance, the administration of the wrong blood product to patients. The system presents real-time insights in patient flows, blood products and equipment use. The data stored and collected during the pilots were the basis for deriving information on the usefulness of RFID and the assessment of the accuracy and completeness of the collected data. Besides the functionality that was used in the pilot at the Academic Medical Center, Geodan Movida offers a portfolio of location, identification and RFID services for healthcare, such as:
By combining the processed ID and location data of patients, blood products and disposables, patient safety and the efficiency of these processes can be improved. For instance, personnel at the operating room are warned when a blood product might be administered to the wrong patient. Second, hospitals can register the use of disposable material and equipment per patient automatically and more accurately. This also induces a variety of new possibilities on the level of the individual patient. Within the pilot, special care was taken of electromagnetic interference of RFID equipment on medical equipment. Strict tuning and organisational measures are needed to establish an infrastructure that does not cause interference but at the same time provides complete and accurate RFID data processing.
First, all medical equipment that could be influenced by the electromagnetic fields broadcasted by RFID was tested for electromagnetic interference by RFID. Second, the adjustment of the radio fields of, especially the active RFID infrastructure is important. When readers or antennas are too close to each other tags can be picked up by several readers simultaneously and might produce wrong information, like the wrong location or otherwise. Besides these technical challenges other points of interest are education of users, a clear insight of the processes that will be supported by RFID and privacy issues.
RFID can provide tangible benefits in the healthcare industry especially when it comes to: