
The challenge for the 21st century anaesthesia leaders will be to bridge the widening gap in practice and education within the speciality whilst at the same time increasing its safety.
Anaesthesia and its practice has developed enormously following WW II, thanks to an explosive growth of anaesthesia equipment and tools, shorter acting drugs, electronics and sophisticated monitoring equipment. Anaesthesia education, training and licensing has not grown at the same pace, certainly not globally. In the last two decades, anaesthesia in the more affluent world has further evolved into perioperative medicine, the practice thereof is still emerging1. The challenge for the 21st century anaesthesia leaders will be to bridge the widening gap in practice and education within the speciality whilst at the same time increasing its safety.
The first Harvard Medical Practice study demonstrated a substantial loss of resources (taxpayers money) by medical negligence and errors whilst awareness about this seemed low or absent amongst practising professionals2. To Err is Human emphasised that safety and quality of care of the patient should be underpinned by improving standards and incorporating safety in training, education and maintenance of registration3 4 5. The Joint Learning Initiative not only revealed a worldwide physician shortage but also discussed and advised on how to overcome this obstacle6.
The World Health Organisation made patient safety a number one priority. The awareness and emphasis on patient safety and quality of care have focused attention on developing different approaches to training (skills), education (knowledge) and competencies (attitude) required for the safe practice of medicine in general and in anaesthesia specifically.
Since the successful public demonstration of anaesthesia (1846) in Boston, USA and the comment made by the surgeon in charge: “Gentlemen, this is no humbug”, dentists, physicians and paramedical cadre have mastered the technique to render patients unaware of the detrimental effects of surgical or other, less invasive procedures.
 The first administrations were mostly done by physicians. Physicians administered anaesthesia In the Anglo-Saxon influence sphere, some as specialists some as general physicians whilst on the American and European mainland, surgeons often induced anaesthesia and then handed the care over to an assistant supervising the anaesthetic. Hence, the contemporary administration of anaesthesia is practised by a variety of trained individuals around the world.
The first administrations were mostly done by physicians. Physicians administered anaesthesia In the Anglo-Saxon influence sphere, some as specialists some as general physicians whilst on the American and European mainland, surgeons often induced anaesthesia and then handed the care over to an assistant supervising the anaesthetic. Hence, the contemporary administration of anaesthesia is practised by a variety of trained individuals around the world.
Surgeons, cardiologists and radiologists were able to develop new techniques through the serendipity of inventive, creative and persistent anaesthesiologists to adapt and adjust to new circumstances in the best interest of the patient and in close cooperation with technicians, pharmacists and engineers. Non-physician anaesthetists have mostly concentrated on care rather than on the cure of the patient and always required a formal prescription - in the widest sense of the word - of the administration of anaesthesia by a physician.
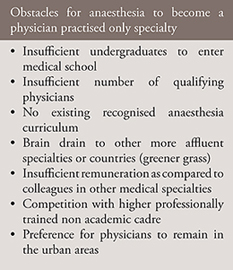
The introduction of anaesthesia as a physician practised only speciality world wide has met with a number of obstacles such as described in table-17 8. All of these are the result of a global physician workforce shortage but why is anaesthesia more affected than other specialities such as radiology or surgery? Radiologists cannot function without adequate and well-maintained equipment and assistance and will therefore rarely flourish in the district hospital. However, a radiographer can take simple X rays that the district physician can use in their practice. The same is true for anaesthesia: with simple means basic anaesthesia can be administered. It does not require a specialist, a general physician or an assistant thus trained can safely administer. However, this mode of practice will not facilitate difficult cardiac surgery or safe anaesthesia for a 63 year old cardiac compromised patient with diabetes and hypertension for a cholecystectomy. History in the more affluent world has shown that a critical mass, a core of dedicated, enthusiastic individuals is required to further improve the quality of care in the speciality establishing the speciality in its full breadth. Moreover, advances in surgery and its outcome are inextricably linked and influenced by the quality of anaesthesia care and cure. Additionally, populations are ageing demanding regular orthopaedic, plastic, transplant or oncology surgery. Moreover, younger physicians do not wish to work the same number of hours commonly practised in the recent past by their predecessors7 9 .
These factors have opened the floor to develop and strengthen non-physician anaesthesia training and practice, filling the void. Evidence-based planning, decision making and re-assessing the process of recruitment, training and re-registration of anaesthesia providers are urgently required.
The scope of anaesthesia
Anaesthesia has become an integral part of the practice of perioperative medicine. Not only surgeons have come to realise that good anaesthesia improves the surgical outcome, psychiatrists prefer anaesthetists to look after the vital functions of their patients during Electro Convulsive Therapy. The list of physicians whose patients need anaesthesia is too long for an individual call out; just rest assured that all doctors aim to keep their patients in optimal condition whilst undergoing any procedure. Perioperative medicine encompasses perioperative care from pre-operative assessment until discharge from the hospital. The different phases are:
As more and more medical practitioners require safe sedation and anaesthesia for their patients, anaesthesiologists are in much more demand and particularly more outside the operating room. Quality of anaesthesia providers must not be sacrificed on account of increased need.
How to cope with a growing demand for the speciality
Several stake holders play a role in providing solution to this problem. Having adequately trained professionals providing anaesthesia is important to patients in the first place. They would like to sustain their surgery with minimal side effects followed by a speedy recovery. Secondly, physicians and other para-medical cadre aiming to practice anaesthesia as a career need an appropriate curriculum, qualification and registration in order to practice safely. Lastly, government is not only charged with the control of training programmes but at the same time committed to improve the quality of care for patients nationwide at all levels: rural, district and central.
A first step for all parties involved is to agree on who may practice anaesthesia under which conditions. An anaesthesiologist is a physician further trained as a medical specialist who masters all aspects of cure and care at the conclusion of their training10 11 . Certain aspects of perioperative medicine can be delegated - in some parts of the world - under clearly described conditions and limitations to para-medical trained personnel. These individuals function as the extended arm of the physician, preferably an anaesthesiologist. Education and skills training should be based on close cooperation with physician anaesthesiologists. Therefore, a national curriculum, with set standards both of training and examinations must be agreed on. Following ongoing assessment and maintenance of a logbook, further enhances the high standards. In some countries, re-certification and re-registration have already found a place such as is commonplace in aviation.
Who should train the future anaesthesia administrators
The medical background of the anaesthesiologist is essential to comprehend the full picture of disease, possibilities of treatment and quality of long-term cure and care for the patient. Anaesthesiologists must naturally contribute to the education of the non-physician anaesthetists. This is however not common practice in the world. Some medically trained colleagues feel able to teach or supervise the administration of anaesthesia. Regarding this practice, let it suffice to have a surgeon speak: Robert Monod was a surgeon and the chairman of the international congress preparing the foundations of the World Federation of Societies of Anaesthesiologists (WFSA): “It is time anaesthesia freed itself from the tutelage of surgery” were the words he said at their opening ceremony in 1951. His words became reality when WFSA saw its inauguration on 9th of September 1955 adopting as their motto: to make available the highest standards of anaesthesia, pain treatment, trauma management and resuscitation. To make anaesthesiologists responsible of delegating their responsibility and set the standards of those professionals, that seems to follow naturally.