
Cardiovascular Diseases have grown to epidemic proportions in India leading to high mortality. Apollo Hospitals and Microsoft have come together to develop and implement a model using Artificial Intelligence (AI) and Big Data to help us define risk prediction, create stratified populations and build targeted therapies and treatment, thereby avoiding preventable deaths.
Cardiovascular diseases have grown to epidemic proportions in developing countries such as India, where lifestyle patterns have changed significantly due to growing urbanisation, dietary habits, reduced physical activity, and associated psychological stress. Currently, cardiovascular diseases contribute to more than 29 per cent of deaths, while Coronary Heart Disease alone contributes to around 15 per cent of deaths in India. Though, there have been multiple studies on cardiovascular disease risk factors since early 1940s, they were not specifically applied to Indian population with high accuracy. Further, most of these studies had selection bias in terms of choosing the risk factors and wouldn’t provide a prospective feedback loop to account for a Cardiovascular event in an individual on a future date.
Apollo Hospitals and Microsoft have joined hands to develop the Standard Cardiovascular Risk Score in Indian population based on the available data at Apollo Hospitals using AI and Machine Learning (ML). The basic objective of this unique initiative is in developing a more accurate risk prediction model so that in conjunction with screening, diseases can be averted in high risk groups.
The study started with the analysis of over 400,000 individual health check records that were collected between 2010 to 2017 from six centres of Apollo Hospitals and matching them with 60,000 patients with discharge summaries of cardiovascular events. All the records were anonymised by removing patient name and unique identification number. Following the data hygiene and curation, the initial model was built on approximately 7,000 patients with cardiovascular Event discharges and a previous health check record (Cases) with 25,000 individuals who had two or more health checks done in the same period without any cardiovascular event (Controls).
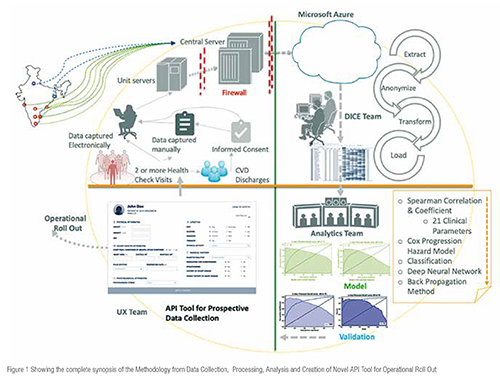
Health check data yields more than 100 clinical parameters for each individuals. The initial step was to filter and identify the applicable risk factors. As the next step, Spearman’s correlation coefficient was used to correlate risk factors to a cardiovascular event. The data was filtered with respect to all the parameters and were further grouped and normalised. After the clinical validation process, around 21 clinical risk factor was selected for further study and validation.
Hazard models were used to predict time to event; these models were built to have unique advantage over regression model to further improve accuracy. Applying the recent advances on Deep Learning on Survival Analysis, we could create an integrated model which provided improved inferencing of co-variate (Hazard Model) while giving better prediction score (Deep Learning).
The accuracy of the model looking at the 21 clinical risk factors stands at the AUC 0.83 which is significantly higher than Framingham Risk Score for the same population at AUC 0.47. One of the significant outcomes was about determining the cardiovascular risk in younger (below 40 years) population (16.6 per cent).Secondly, the interplay of multiple factors were more significant than any one individual factor. For example, the study yielded higher correlation between hypertension and diabetes as risk factors for cardiovascular event than any one of the factors individually. The study also highlighted that the higher diastolic blood pressure is a better indicator of cardiovascular disease than higher Systolic Blood Pressure, particularly in a younger population. Specific to Indian population, chewing tobacco is more harmful than smoking for cardiovascular disease (around 7 percentage point more). Lastly, higher BMI (> 27) with either smoking or chewing tobacco increases heart risk by 14 per cent percentage point.
The results of the study were next validated retrospectively with blinded data set from 2 other (larger) centres of Apollo Hospitals with AUC scores of 0.844 (n = 2389) and 0.92 (n=857). During this validation process, another significant inference came out in the form of frequency of health check to the accuracy of prediction. The study concluded that when the health checks are done more frequently, the accuracy of the prediction improves providing a better predictability for cardiovascular event.
With the technology capability developed and promising initial results of the retrospective study, the Apollo Hospital: Microsoft Team next focused on deploying the AI model into the organisational Electronic Medical Records (EMR) for improved adoption. A roadshow programme for eight Apollo Hospitals and a prospective longitudinal study with ten Indian Hospitals (including reputed academic institutions) were subsequently designed. The next objective was to focus on empowering physicians to determine risk factors in patients with more holistic way and provide insights to them for lifestyle modification and timely interventions.
a) Integrating the AI model as an API to the organisational EMR:
The programme was built through novel ideas and designing of the operational processes. The API tool is built for the EMR, where the patient’s current risks are determined and methods to reduce risk were provided during the discussion with the physician. There are currently no existing tool based on computation on deep neural networks available to predict cardiovascular risks.
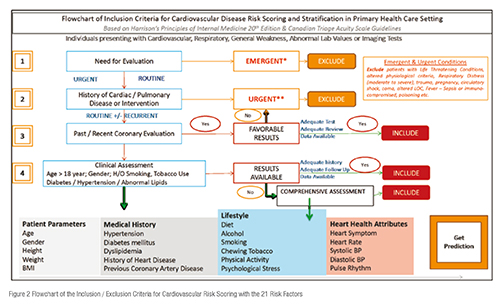
Next step in the workflow was to define the inclusion and exclusion criteria as under what clinical condition a physician can choose to generate the risk score of an individual or a patient.
Following the development of the inclusion criteria, the team designed the work flow required to implement the process and integrating the API at personalised health check clinics in the hospitals and Apollo Clinics; Specialty Clinics like Apollo Sugar and Healthy Heart Clinics; Physician OP Clinics in Internal Medicine, Cardiology etc; and finally, developing an App for Peripheral Public Camps and Remote Care – Apollo TeleHealth.
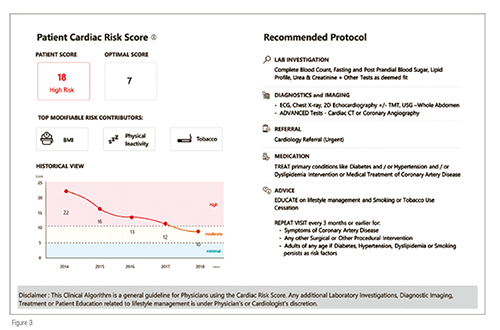
In all of the above situations, the patient- / individual-related clinical data is collected in the EMR which would auto populate the cardiac risk score user interface. On clicking the ‘Get Prediction’ button, the Cardiac Risk Score is generated with the following features: (Figure 3) –
• The risk score of the patient with the optimal score for his / her age.
• The top three modifiable risk contributors, which the patient should work on moving forward to reduce the risk of the cardiovascular disease.
• The patient’s historical risk score that has been generated from the earlier health checks done in the system, which predicts the risk trend.
• The clinical decision support system which provides what the physician should direct the patient towards next lab investigations, Diagnostic imaging, referral to cardiologists, medications, patient and family education and repeat visit timelines.
• A legal disclaimer such as: This clinical algorithm is a general guideline for physicians using the cardiac risk score. Any additional laboratory investigations, diagnostic imaging, treatment or patient education related to lifestyle management is under the physician’s or cardiologist’s discretion.
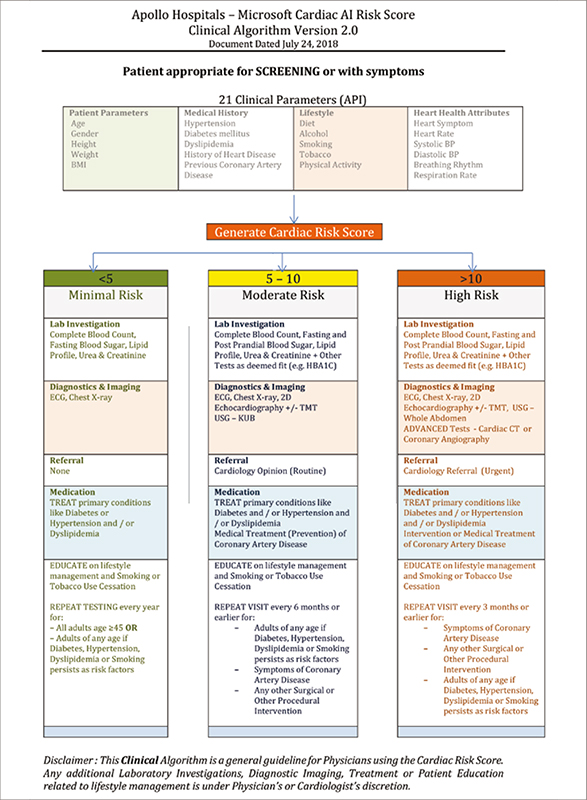
b) Clinical Decision Support Systems
One of the key imperatives for any clinical AI programme is to provide a link between the AI–ML research and integrate this with core clinical functionality for a better adoption of clinicians. The clinical algorithm was developed to support the patient’s risk score and channelise them through appropriate care processes as described above. Figure 4 shows the process. The benefit of the clinical algorithm were two-fold:
• It provided an immediate and handy guideline for the next course of action for the patients with high risk to seek next level of intervention
• It standardised the process of the investigations and referral thereby helping the physicians to guide their patients better
• Prospective Study & Roadshows with Clinicians
For the prospective use of the cardiac risk score API tool, the team designed an observational prospective study with appropriate layers of informed consent, data security &confidentiality and applied to 10 institutional ethics committees across the country. Currently, approvals have been obtained for the prospective studies which are underway for further validation and calibration. Similarly, premier healthcare institutions outside India in USA, Europe and Canada are being brought in to make an international data consortium to take the cardiac AI risk score, for global population with multi-ethnic and crossgeographic boundaries. Technically, the opportunity remains to comply with national and international data privacy laws and integrate the API with translatable interoperable EMR / EHR systems.
In the context of rolling this out to clinicians during the roadshows, the team adopted three fundamental principles:
1. Algorithm + Clinician: AI algorithms are not replacements for clinicians, but rather are complementary to clinician decision–making
2. Risk Identification and Prevention: This tool does not diagnose coronary artery disease;it provides a risk computation for mitigation and prevention only.
3. For Outpatient and Health Check Clinics: The tool has been prepared for use at preventive cardiology screening programmes at the outpatient clinics and for health check clinics.
The roadshows in August 2018 and January 2019 covered 600 Physicians and 100 cardiologists at eight Apollo locations.
Conclusion
Beginning with an unmet need to standardise a cardiovascular risk score for Indian population, this endeavour looks forward to involve healthcare institutions, public and private health services, corporate wellness programmes, e–Health portals etc., across geographies and multiple ethnicities to use the risk score API. The personalised output and recommendations of the risk score algorithm will benefit both the physicians and the people to prevent cardiovascular events in the long-run.