
Collaboration and communication among all the team members of the Intensive Care Unit (ICU), where patient activity is high, goes a long way in promoting effective care of critically ill patients.
Collaboration between physicians and nurses is an important component of effective care in the hospital setting. When working together toward common goals, collaboration has been identified as a way of improving care for the critically ill patients as it enables input from the multidisciplinary team members in promoting decision-making based on more useful information1 . Patient care depends on the interactions of various providers, especially in the Intensive Care Unit (ICU), where patient acuity levels are high and critical illness states often result in sudden changes, some of which are life-threatening. As a result, collaboration is vital in ensuring appropriate care and treatment of the critically ill patient.
The importance of collaboration and communication and its impact on patient outcomes in the ICU is well recognised by many national and international organisations. The Joint Commission, the American Association of Critical Care Nurses, the Society for Critical Care Medicine and the National Institutes of Health have previously advocated for interdisciplinary communication and collaboration for patient care in the ICU2,3,4 . Recent recommendations from the American College of Chest Physicians and the American Association of Critical Care Nurses also focus on the importance of skilled communication and true collaboration as essential elements for transforming work environments5 . The Society of Critical Care Medicine's clinical practice guidelines for patient-centered care in the ICU advocate for communication and shared decision-making to enhance care for the critically ill patient6 . Most recently, the results of a critical care consensus initiative identified that improving communication among providers and formal training on the interdisciplinary team model are advocated to improve the management of ICU services7 . As communication and collaboration are essential to patient-focussed care, open communication and interdisciplinary collaboration are key components in achieving patient-centred care and meeting patient care goals5.

Clinical practice guidelines for patient-centered care highlight that collaboration, good communication skills and conflict management skills are needed for the shared decision making1, model to be effective in the ICU. Characteristics of collaboration include collegiality, communication, cooperation, mutual trust, respect and shared decision-making (Table 1). Research has demonstrated associations between increased nurse-physician collaboration and lower risk of negative patient outcomes including lower risk of re-admission to the ICU and risk-adjusted mortality1,8,9 . In a series of prospective multisite studies, Shortell10 , Knaus11 , and Zimmerman12 and colleagues demonstrated that organisational characteristics including communication and collaboration influenced patient outcomes. In examining characteristics of effective care in the ICU in 17,440 patients across 42 ICUs, Shortell and colleagues10 found that caregiver interaction including leadership, coordination and communication was significantly associated with lower risk of adjusted length of stay (beta=.34), lower nurse turnover (beta=-.36), higher evaluated technical quality of care (beta=.81) and greater evaluated ability to meet family members needs (beta=.74)10. In a sample of 3,672 ICU admissions involving 316 nurses and 202 physicians, Zimmerman and colleagues demonstrated that superior organisational practices among ICUs with increased risk-adjusted survival were related to a patient-centered culture, strong medical and nursing leadership, effective communication and coordination and open, collaborative approaches to solving problems and managing conflict.
Additional studies have found significant associations between the use of effective multidisciplinary rounds13 and collaboration. In a study assessing the impact of an intervention focussed on improving communication and collaboration in the ICU which included daily multidisciplinary rounds, the addition of a nurse practitioner and the appointment of a hospitalist medical director to oversee patient care, increased collaboration. This is attributed to the interactions of the nurse practitioner with medical and nursing staff along with multidisciplinary rounds . The use of a daily goal sheet in rounds can be a useful adjunct to promote awareness of the patient care goals as well as to promote improved communication and collaboration in the ICU. In using a goal sheet on daily rounds, the patient care goals for the day can be discussed and areas that need addressing can be easily identified. For example, ventilator weaning goals, nutritional goals, medication changes, consultations, family communication and other aspects of care can be discussed among the team to clarify the focus of patient care for the day. Use of the daily goal sheet promotes collaboration among the ICU team members as it establishes priority areas of patient care and promotes further discussion throughout the day with updates for team members. In working to achieve the patient goals identified in the daily goal sheet, ICU team members further collaborate to meet those goals.
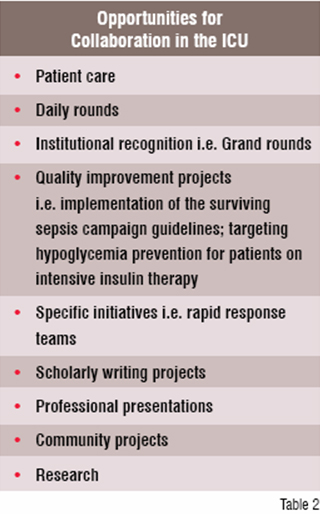
A number of opportunities have been identified for improving collaboration in the ICU including participation of the multidisciplinary team in grand rounds, research and quality improvement initiatives (Table 2). Rapid response teams are one specific example of an institution-wide initiative that promotes collaboration among the ICU team members who serve as responders. Forming multidisciplinary teams to address clinical issues, formulating new protocols, or implementing best practices help to promote collaboration among the ICU team members. Specific examples of initiatives include forming a committee or task force to focus on sepsis identification, management, and implementation of the Surving Sepsis Campaign Guidelines, targeting hypoglycemia prevention for patients on intravenous insulin protocols, or promoting palliative care consultations in the ICU. Conducting research in the ICU offers additional experiences to promote collaboration among the ICU team. Other opportunities including publications and presentations of ICU team initiatives at local, regional and national forums, also promote collaboration among the ICU team members.
Multidisciplinary collaboration in the ICU is vital in ensuring appropriate care and treatment of the critically ill patients as well as an important component of establishing and meeting patient care goals. Collaboration should be encouraged and promotedon the ICU team as it is an essential component of high performance and helps to promote best patient outcomes.
1 Baggs JG, Schmitt MH, Mushlin AI, et al. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Crit Car Med 1999;27:1991-1998.
2 National Institutes of Health. Consensus conference critical care medicine. JAMA 1983;250:789-804.
3 Joint Commission on Accreditation of Hospitals. Accreditation Manual for Hospitals. 2007; JCAHO Chicago IL.
4 American Association of Critical Care Nurses. Collaborative Practice Model: The Organization of Human Resources in Critical Care Units. AACN: Newport Beach CA
5 McCauley K, Irwin RS. Changing the work environment in intensive care units to achieve patient-focused care: the time has come. Am J Crit Care 2006;15:541-548.
6 Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Car Medicine Taskforce 2004-2005. Crit Care Med 2007;35:605-622.
7 Barnato AE, Kahn JM, Rubenfeld G. et al. Prioritizing the organization and management of intensive care services in the United States: The PrOMIS Conference. Crit Care Med 2007;35-1003-1011.
8 Baggs JG, Ryan SA, :Phelps CE, Richeson JF, Johnson JE. The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart & Lung 1993;21:18-24.
9 Baggs JC, Ryan SA, Phelps CE, et al. The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung 1993;21:18-24.
10 Shortell SM et al. The performance of intensive care units: does good management make a difference? Medical Care 1994;32:508-525.
11 Knaus WA, Draper EA, Wagner DP, Zimmerman JE. An evaluation of outcomes from intensive care in major medical centers. Ann Intern Med 1986;10:410-418.
12 Zimmerman JE et al. Improving intensive care: a prospective, multicenter study. Crit Care Med 1993:21:1443-51.
13 Vazirani S, Hyas RD, Shaprios MF. Cowan M. Effect of a multidisciplinary intervention on communcation and collaboration among physicians and nurses. Am J Crit Care 2005;14:71-77.