
The field of complex congenital heart disease has evolved greatly, allowing more patients to survive into adulthood. Their healthcare issues are multi-faceted, mandating a multi-disciplinary approach. Forward planning and resource allocation for manpower and infrastructure development, based on accurate demographic data, will undoubtedly help countries face this growing challenge.
According to the World Health Organization (WHO), a well-functioning healthcare system requires a robust financing mechanism, a well-trained workforce, and importantly, reliable information on which to base decisions and policies. The knowledge of adult prevalence of congenital heart disease can estimate the need for specialised services. As the field of congenital heart disease matures, we are beginning to recognise a new era of changing demographics that must be matched with services and infrastructure that commensurate with its growth.
The annual worldwide birthrate of 150 million births during the 1990 had already corresponded to 1.35 million live births with CHD every year. With advancements in pediatric cardiac care and improvement in socio-economical circumstances in developing countries allowing for an increased survival of these patients into adulthood, the burden of adult congenital heart disease is only expected to grow. By the beginning of the 21st century, adult survival is expected to reach 75 years. This is an increase of 15 years as compared to the period of 1987 to 1993. In Ireland, the percentage of CHD patients surviving into adulthood is over 90 per cent.
Where previously scant, empirical and contemporary data is now available on the epidemiology of CHD in the general adult population. This landmark paper published in 2007 had characterised the problem, incidence, prevalence and distribution of adult congenital heart disease in the province of Quebec, Canada. It helped inform public health research, priority setting and program monitoring. In this population wide study, severe lesions accounted for 9 per cent of the CHD population. The median age of all patients with severe CHD was 11 years (interquartile range, 4 to 22 years) in 1985 and 17 years (interquartile range, 10 to 28 years) in 2000 (p < 0.001). The prevalence of severe CHD increased from 1985 to 2000, but the increase in adults was significantly higher than that observed in children, suggesting that this population has yet to stabilise. In addition, in the year 2000, there were nearly equal numbers of adults and children with severe CHD.
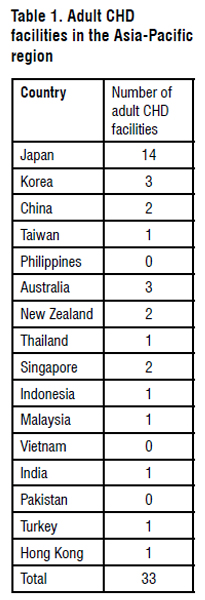
Asia reported the highest CHD birth prevalence with 9.3 per 1000 live births (95 per cent confidence interval: 8.9 to 9.7), with relatively more pulmonary outflow obstructions and ventricular septal defects. In Japan, based on the death certificates of CHD registered with the Japanese government, a total of 622,800 patients (49 per cent were children and 51 per cent adults) were estimated to be alive in 1997. From 1997 to 2007, there has been an estimated increase of 9,000 adults annually, with 454,000 adults estimated to be alive in 2013. Likewise, adults made up a substantial proportion of the total CHD population in Korea (22-26 per cent), Taiwan (20 per cent), and Thailand (32 per cent). Adults with CHD of moderate or greater severity made up 36.6 per cent and 32 per cent of patients in Korea and Japan, respectively. In Singapore, the number of adults with CHD (about 15,000) was higher compared with children with CHD (about 5,000) in 2008. This trend of increasing adult CHD patients in the Asia-Pacific region mirrors what has been observed in North America and Europe.
Mortality rates in the CHD population in Quebec, Canada, were noted to have decreased in all age groups below 65 years during July 1987 to June 2005. The largest reduction was noted in infants with a mortality rate ratio of 0.23. In adults between the ages of 18 and 64 years, the mortality reduction was similar to that of the general population with a rate ratio of 0.84. The differences in mortality between the industrialised and third world countries are striking: from 3-7 per cent to 20 per cent respectively. Furthermore, the mortality from CHD is likely under-reported in third world nations because access to diagnosis is more difficult, and the great majority of studies only report data from patients in tertiary centres.. In addition, a difference in mortality due to CHD is also seen between different socio-economic groups in developed countries. For instance, an analysis of death certificates by the Centers for Disease Control in the United States has shown that mortality from CHD is generally higher in blacks than in whites, despite the incidence of CHD being slightly lower in the former per cent.
CHD patients are at increased risk for chronic renal disease, epilepsy, stroke, transient ischemic attack, secondary erythrocytosis, diabetes, hypertension, heart failure and cancer. Atrial arrhythmias occurred in 15 per cent of adults with CHD. The lifetime incidence increased steadily with age and was associated with three times the risk of cardiac intervention, a doubling of the risk of adverse events, and a near 50 per cent increase in mortality. A diagnosis of pulmonary hypertension in adults with CHD is associated with more than double the risk for all-cause mortality and a three times increase in health services utilisation (inpatient and outpatient service, such as cardiac catheterisation and coronary / intensive care hospitalisation), reflecting a high level of morbidity. The need for valvular interventions has also increased from 42 per cent to 63 per cent in the last two decades in CHD patients. The complexity of the cardiac anatomy and the myriad of problems associated with this group of patients mandates that this growing burden must fall on the shoulders of a multi-disciplinary team led by qualified adult congenital heart disease specialists.
Country by country, life expectancy will eventually follow a path of uninterrupted but slowing increase. Asian regions will grow fastest to the west, slowest to the east, but in every case with growth rates, at least up to 2100. Between 2100 and 2300, the proportion of world population 65 years and older will increase by one-third; the proportion 80 years and older will double, and the proportion 100 years and older will increase by nine folds. Afilalo et al. described the geriatric CHD population in the Quebec population from 1990 to 2005. The prevalence of CHD in older adults was about 3.8 per 1000 indexed to the general population.
The distribution of lesions in the adult CHD population varies, depending on the location where the proportions are taken, as well as the age group concerned. Patients with severe lesions made up about 9 per cent of the CHD population in Quebec, Canada. In the geriatric age group, the most common types of CHD lesions in older adults were shunt lesions (60 per cent), followed by valvular lesions (37 per cent) and severe CHD (3 per cent). Type of CHD and CHD-related complications had a minor impact on mortality, which was predominantly driven by acquired co-morbid conditions. The most powerful predictors of mortality in this age group were dementia, gastrointestinal bleed, and chronic kidney disease.
The financial burden of congenital heart disease is receiving increasing attention. Garson et al. described a multi-center assessment of lifetime cost of care for children with CHD in 1994. Average charges of care from birth to 40 years of age varied from US$ 47,515-73,606. Services included in this study were that of routine clinic visit, complex clinic visit, hospital admission for medical admission, hospital admission for surgical treatment, hospital admission for interventional treatment, hospital admission for pacemaker implantation, and number of years the patient has taken cardiac medication. It however does not take into account non-cardiovascular care for these children, cost to the family (loss of income for parents, costs of uncovered medical services and drugs, costs of psychologist). Also not included are societal costs associated with loss of work, increased healthcare needs, and increased educational services. In contrast, updated data on hospitalisations for individuals with congenital heart defects in the U.S. in 2004 were about US$1.4 billion, and severe CHD defects accounted for about US$511 million (18), or about 37 per cent of the hospital cost associated with CHD defects. In 2005, for privately insured population in the U.S., estimated medical care costs for an infant with any CHD defect was merely US$100,000, and costs were higher for those infants with a severe CHD defect. We can only expect this cost to further increase in time to come.
Hospitalisation rates for patients with CHD were higher than the general adult population in Quebec (relative risk of 2.08). In addition, patients with severe CHD have higher adjusted rates of outpatient cardiologist care, emergency department utilisation, hospitalisation and days in critical care than patients with other congenital cardiac lesions. In Singapore, CHD patients were found to not only require longer length of hospital stay for both cardiac and non-cardiac related medical conditions, but also required interdisciplinary resources.
Life insurance remains an important component of financial planning. Despite recommendations from cardiac societies, availability of insurance varies considerably not only between but also within countries, with surprising discordance between insurance policies and available outcome data. Health insurance, in particular, may exclude treatment for the cardiac condition in certain countries. In Germany, one survey found that more than 30 per cent of CHD patients were refused life insurance. The U.S. had taken the lead by passing the Patient Protection and Affordable Act in 2010, alleviating the unfair discrimination that besieges CHD patients. Singapore, in its recent revision of its policy from March 2013, has also taken a step forward by extending its nationwide insurance to include newly diagnosed CHD and neonatal conditions. With such sterling examples, this should be a consideration for countries when formulating their healthcare policies.
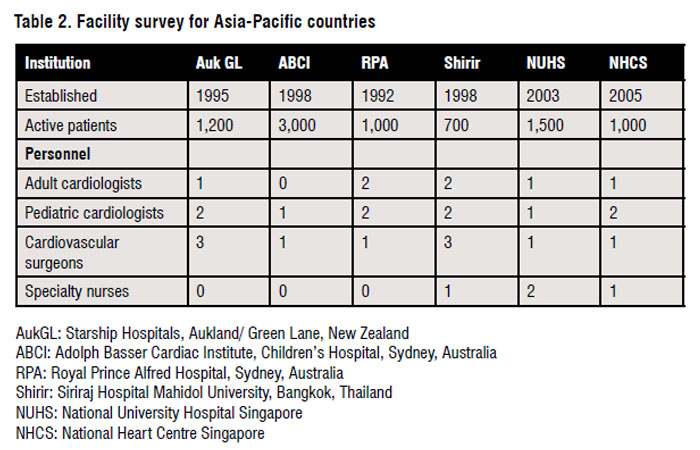
A strong relationship is a must between the paediatric cardiologist and adult congenital heart disease specialists to ensure a smooth transition of the patient to adult care. This relationship, in addition to suitable policies, will prevent a gap of care should the patient be lost to follow up. In Quebec, Canada, for example, law mandates all paediatric cardiologists to transfer the care of their patients to an adult institution by the age of 18. Predictors of lack of cardiology follow up in adulthood included male gender, non-severe lesions, and a history of follow up outside a university hospital setting. Improved communication with primary care physicians may reduce the proportion of patients lost to cardiac follow up. More trained imaging specialists are needed in the field of echocardiography, computed tomography and magnetic resonance imaging to achieve accurate diagnoses, and guide treatment. The impact of the increased use of fetal echocardiography and pregnancy termination on reduction of CHD birth prevalence is expected in the next time period. Intervention will need to be executed through the hands of experienced interventionists and cardiothoracic surgeons, who are familiar with the peculiarities of complex CHD. Cardiac chambers often enlarge and arrhythmias are more common. Ventricles tend to develop systolic dysfunction, resulting in the main causes of death as that of progressive heart failure and sudden cardiac arrest. This brings in the heart failure team and the electrophysiologists. Patients with unrepaired complex cyanotic congenital heart disease are repeatedly advised to avoid pregnancies, given the extraordinarily high risks to both mother and the child. The obstetrician and gynecologist are needed to counsel on contraception and surrogacy. The need for screening any patient should be individualised based on type, likelihood, level of potential exposure, as well as time of gestation during which the exposure had occurred. It is also important to include the obstetric history. If and when they do get pregnant, we need them to run the high-risk pregnancy clinics in tandem with the congenital heart disease specialists. They will need to tackle issues on whether to terminate the pregnancy or continue with a clearly defined plan worked out with the anesthetist and the intensive care team.
A dedicated nurse is needed to educate the patient and their caregivers about the disease, how to cope with their disabilities and ensure that they remain within the healthcare system and are not lost to follow up. Add on the fact that these patients frequently suffer from emotional and psychological trauma associated with the high level of anxiety about the underlying heart condition and prognosis, difficulties with social interaction, specific issues about employment, insurance and physical activities and poor self-esteem, psychologists and medical social workers will be needed to act as advocates for the patients who may face unfair discrimination.
Promoting multicenter research remains pivotal to fill the growing knowledge gaps. Epidemiology, outcomes research and genetics are rapidly advancing. Multicenter registries will allow for further prospective and retrospective studies to be done. Patient-centered care and education involves not only learning more about each diagnosis of CHD that we have, but also refining and adding to the current pool of knowledge. This can only be achieved through research.
There is a need to teach fellow healthcare workers and the public about the disease as well as the avoidance of risk factors for CHD. Known risk factors include maternal pre-gestational diabetes mellitus, consanguineous marriages, phenylketonuria, febrile illness infections, various therapeutic drug exposures, vitamin A use, marijuana use, and exposure to organic solvents.
The high total CHD birth prevalence found in Asia could partly be attributed to high consanguinity rates in some study populations. CHD birth prevalence amongst children with consanguineous parents was found to be considerably higher than in non-consanguineous parents, suggesting an important genetic influence. Data about alcohol usage, hard drugs or cigarette smoking during pregnancy are insufficient to determine risk for CHD. More research is required in this area.
Inclusion of next of kin and family may allow for better continuity of care and follow up. The patient must be empowered to be involved and in charge of their care, and thereby giving advanced directive in their overall healthcare plan. Support must also be given for the caregiver to reduce the incidence of caregiver fatigue. For patients with unrepaired complex disease, the congenital heart disease team should broach the idea of palliation to prepare the patient and their family at the appropriate time. This care is shared with the palliative care team so that the patients can face the burden of their illness and possible demise with dignity.
Access to healthcare across countries, groups and individuals, is largely influenced by social and economic conditions as well as the healthcare policies in place. Countries have different policies and plans in relation to the personal and population-based healthcare goals within their societies. The exact configuration of the healthcare system varies from one country to another. One of the more recent CHD studies in Thailand reported 0.41-1.05 prevalent cases of unrecognised CHD for every 1000 elementary-age students. This variation was due to the topography and the limitation of medical staff and facilities in the study area. In a recent study in Mozambique, a pattern of late presentation accompanied by high rate of complications was found. Of the 534 CHD patients studied, about half were diagnosed after the age of two. Preventable complications were present in 29 per cent at the time of diagnosis. All references are available at www.asianhhm.com