
Most infectious and chronic diseases have a common ground – our basic environment and life force. A lot of infections start off as one but steadily lead to chronic conditions in absence of basic amenities, proper healthcare facilities and treatment protocols. As 2020 has gaped open many wounds, it seems like prevention and wellness has to be the new normal in healthcare.
COVID-19 has exposed the health quotient of countries and geographies, the basic civic sense of the populace, the healthcare infrastructure, the political saga and our susceptibility to economic distress. It has also exposed the pollution levels caused by urbanisation thus exposing effects on health. Each of these impacts our health – mental, emotional and physical. It is time to pick up the pieces and mend....
Like a serious joke, the pandemic has revealed much more about the status of our health than information about the disease itself. The speed of spread of the disease globally has showcased our susceptibility to infections, to environment, and, to social nuances.49, It has laid bare the ability to deal with
such problems and the catalysing possibilities of more such spreads.
COVID-19 struck at a time when we were still comprehending the effects and work around strategies for chronic diseases, having just transcended the curve for better management of infectious diseases and trying to negotiate the steep rising trend in chronic and lifestyle disease. We were caught unaware by this pandemic, despite the World Health Organization (WHO) warnings. This in the 21st century showcases the fragility and vulnerability of humans this age because of the economic development and ease of geographic transcendence.
Post the COVID-19 infections, it is yet to be ascertained what the aftermath would be – both in terms of chronic extensions of the disease as well as the preventive aspects especially given the virility of the disease.
Whatever the situation be, it is now imperative for us to look at the preventive measures. And these preventive measures cry for care for the environment, for habit, which ultimately forms the base for health, and taking this further from preventive measures to wellness. Not just from the COVID-19 perspective but the overall scenarios in other infectious as well as chronic diseases.
Various surveys across the globe saw people suffering from chronic diseases shy away from hospitals for their regular visits. The numbers we see in our hospitals also tell the same story. However, the turn up in the emergency rooms for critical care by those suffering from chronic conditions has also shown a very steep rise. This indicates that people are ignoring symptoms that can be, and, should be treated early on, preventing the aggression of the disease, choosing instead to stay at home and then turning up when the condition worsens to a level requiring critical care attention.
Another grave and glaring aspect to look at is the effect on the healthcare workers. By mid of September, over 7,000 healthcare workers are estimated to have lost their lives in the pandemic while providing care to those ill and suffering from COVID-19. This pushes us to look at not only infection control preparedness, adherence to processes as well as availability of the required protective gear, but also to have a close look at the health quotient of the healthcare workers themselves. Healthcare workers have a right to safety. Alongside this right, there is a huge responsibility as well – a right to healthy living. But is that possible? Casting an eye to the stressful and long working hours for most healthcare workers, the reason for chronic conditions are fairly apparent. This change needs to start at home.
We need to keep a close eye on these statistics as we re-read and re-comprehend the pre pandemic volumes of infectious and chronic diseases. The numbers resulting from the pandemic are yet to be accounted for. And given the compounding rate at which these could add up along with the aftermath of the pandemic, it is imperative that we create strategies to prevent infectious and chronic diseases from occurring as well as converting to each other. In fact, the larger objective around this should not just be prevention but also to better the health quotient of the general population.
According to the WHO and some publications, it is estimated that about 60 per cent of deaths happen because of chronic diseases and about 32 per cent because of infectious diseases. Again, the pandemic will surely change these numbers. Two decades ago, approximately 46 per cent people suffered from non-communicable diseases, which is expected to have increased to an alarming high of 57 per cent. A lot of data is available to this effect and I do not intend to repeat that here. Reason to stress on this is because it is important to understand that most infectious diseases, if not treated or treated improperly, will lead to chronic diseases. A huge percentage of these are very preventable if we look after our lifestyle and environment – our life forces.
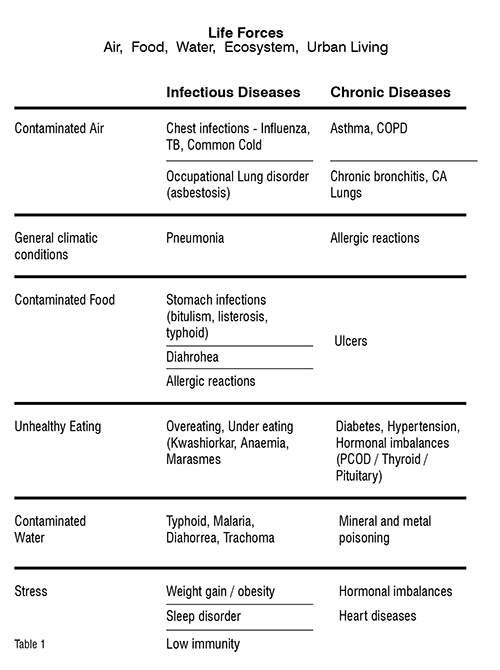
Let us understand some closely knitted basics that are today crying for attention: air, water, food, ecosystem and stressful environment. I would call these our ‘Life Forces’ today. If we take care of these basics, a lot will be taken care of for us in garnering support to reduce the daily concerns of these diseases. Each of these, in deterioration, has cast the net of illness – chronic as well as infectious. The table below attempts to draw out the correlation between the Life Forces and various highly prevalent infectious and chronic diseases. (Table 1)]
In an attempt to prevent further deterioration of the health quotient of the populace, it is imperative to balance out the betterment of the healthcare services with other aspects of basic clean and healthy living viz civic amenities, maintaining the ecosystem and a huge focus on a healthy emotional and mental environment aka stress-free living. The basic civic amenities should provide every citizen potable drinking water, good clean air, and clean (read chemical free) food. While we proudly boast of being born in the 21st century, a proud new generation with many new inventions under our belt, the deadliest of diseases have also been part of that set of inventions. And that is also something that threatens what we so carefully crafted out.
While the same is true in different measures across the world for these factors, a lot needs to be driven on the policy front in India. We have to push this through, and start taking cognisance of the geographicenvironment related health data. We must relate geographic spurts of various infectious as well as chronic diseases to usage of fertilisers and chemicals in farming, for example. Tracing the effects of genetic engineering of food varieties on long-term health effects needs to be checked out. Contaminated water has created havoc in the past and continues to. While we focus diligently on COVID-19, let’s also make a renewed effort to account for the continued number of mortality and cost spend on health issues pertaining to air / water / ecosystem contamination due to unhygienic living, industrial ravages of incorrect waste disposal, even domestic and farming waste disposal. These small measures will go a very long way in bettering the overall health of the nation, safeguarding from the future ravages of disease, enabling better life quality, better economic capability and also a lower health spend. In fact savings from these can actually be ploughed back to create and better the country’s public healthcare system.
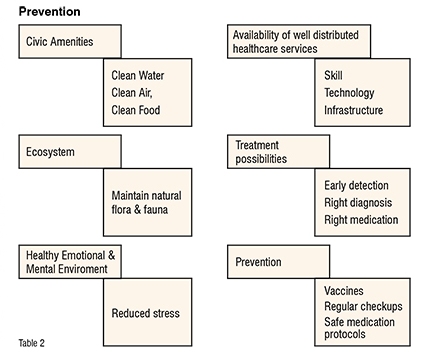
Table 2 on prevention also attempts to specify all that needs to be done on the healthcare side towards treatment as well as prevention of both infectious and chronic diseases. The most important factor being that if services are readily available, those who need those services will definitely reach out there. However, in the rural areas, while the PHCs exist, no doctors or trained staff do, which beats the purpose of the whole situation. The plight of the Anganwadi and Asha workers was laid bare during the pandemic. Clearly the system needs to be strengthened. This strengthening needs multifarious things to be done, including improved education, use of digital aid to overcome skilled manpower availability, a proper digital infra, ensuring each medical pass-out has a compulsory posting in the rural areas, amongst other things. Quality control needs to focus on treatment protocol monitoring closely through digital aids. We also need to ensure that norms for accreditations are the same for both government as well as private hospitals, ensuring that the course offerings and curriculum in medical and nursing education colleges adhere to these norms. Because of these dichotomies, a lot is left wanting. But the good part is that there is something that can be strengthened further.
In a nutshell, we are living in a time where we no longer have a choice to procrastinate about our health. Health can also play a major role in making and breaking economies as the pandemic has shown. Time for us to retrospect, re-invent and work towards a healthier self – individually, statewide, nationwide, and worldwide.