
The healthcare systems in most countries will be rendered unsustainable by the rise in people with long-term conditions like having not just a single disease but multiple conditions. Current strategies will make healthcare unsustainable in all those countries. A model of care and finance to mitigate this problem is outlined.
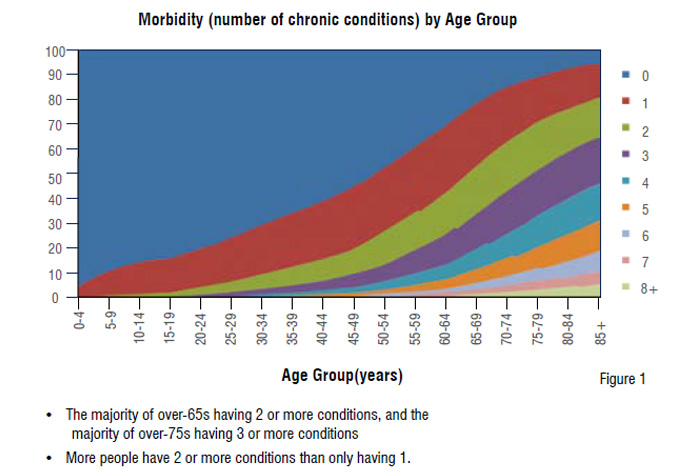
Over the next 40 years, most healthcare systems worldwide face a tsunami of need from people with long-term conditions (diabetes, chronic airways disease, circulatory diseases). There will be a rise of 252 per cent by 2050; the mathematics is inescapable. The majority of people will not have a single disease but multiple morbidity (see Figure 1). In England now, this group of patients use 76 per cent of activity and cost in the health and social care system. They are disproportionately higher users of health services –representing 68 per cent of specialist outpatient attendances, 72 per cent of inpatient bed days, 58 per cent of emergency department attendances, 55 per cent of GP appointments and 59 per cent of practice nurse appointments.
The consequences are equally inescapable for most countries. Firstly, if healthcare systems continue to manage people with Long Term Conditions (LTCs) as they do now, they will not be sustainable. Secondly, the way that a country manages people with long-term conditions will, given the proportion of GDP that this will consume, be a determinant of the competitiveness of that country’s economy. For example, if the U.S. continues its current model of LTC management, and given the built in demographic drivers, by 2065 itwill spend 100 per cent GDP on healthcare. In one sense this is a nonsense statistic. Thirdly, disease specific pathways of care, and hospital-based care are a redundant strategy for the multi-morbidity future. Some countries with a greater balance between ageing and working populations, particularly some in Asia, will fare better, but for everyone status quo is not an option.
Data from the Scottish School of Primary Care’s Multimorbidity Research Programme Guthrie et al. Universally, patients say that they wish to be treated as a whole person and for the health and social care system to act as one team. Despite this, those people who have more than one condition, particularly older people, face a fragmented response. Long-term condition ‘needs’ transcend the organisational boundaries of social, primary, community and secondary care. The current system fragments care for individual patients and this lack of continuity often leads to poorer outcomes and hospital admissions. There now needs to be transformational change in the culture and operating model to ensure a step change in innovation so that healthcare can be a viable entity for the future. That step change is from ‘see, treat and discharge’to‘ identify, integrate care and co-manage’ patients, with technology at the heart of that change.
Model of care
The population care model described below is based on a wealth of international evidence;it has been shown to improve clinical outcomes and to reduce length of stay and unscheduled hospital admissions. The three primary drivers are:
Integrated locality care teams including social care, community services, allied health professionals and general practice
This uses a validated risk profiling tool to support commissioners to understand the needs of the population and manage those at risk. A risk prediction tool will identify patients that are at high and medium to high risk of accessing healthcare services. Targeting the latter with proactive care will assist in slowing disease progression and will allow for interventions to be prioritised. Understanding the population in this way also facilitates the identification of the future resource need and its utilisation. Research evidence shows that 20 per cent of patients identified by risk stratification would not be identified in any other way. This improved access to care for these people has also been shown to improve the quality of outcomes. There are several such tools commercially available. The algorithms are not dissimilar, but there are differences in accuracy and search capability.
Integrated locality care teams including social care, community services, allied health professionals and general practice
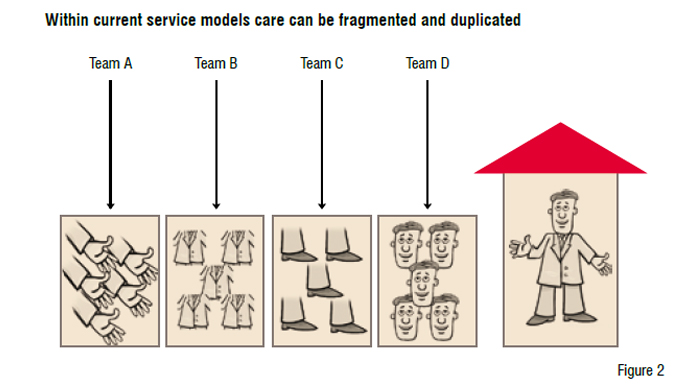
Healthcare systems and mechanisms traditionally focus around the body parts of people for which the different clinicians feel responsible (see Figure 2). This has created fragmentation and duplication, particularly when dealing with people with multiple problems. For the patient it is often just confusing. We also know the outcomes are poorer. The system change that is required is the creation of functionally integrated holistic teams at a neighbourhood level. These teams should include community services, allied health professionals, social care services and specialist nurses and should be linked to the lead clinical provider. The integrated health and social care teams should be based around a neighbourhood (experience suggests a population size of 30,000) to provide integrated and personalised services. Neighbourhood care teams will provide a single main point of contact for patients and carers. Each patient should have a key worker within this team to coordinate their care. Combined with risk stratification, this integrated proactive management of patients will improve their lives. A large randomised trial in the U.S. showed that this sort of approach, for this cohort of patients, resulted in 52 per cent fewer inpatient days, 17 per cent fewer emergency department visits and 49 per cent fewer readmissions. 16 other studies have also showed significant reductions in length of stay, unscheduled admissions and ED attendances.
In the model described here, care is delivered by a multi-disciplinary, prepared and proactive workforce that actively seeks to move patients away from being passive recipients to becoming informed and activated people who are able to co-manage their conditions. Self-management support becomes a clinical responsibility and an integral part of the delivery system, not just an add-on. Professionals can have the view that ‘patients can’t manage their own condition’. The reality is that most people with long-term conditions have to do precisely that for some 7900 hours in a year, and only interact with professionals for an average of 4-5 hours. Unscheduled admissions are often driven by one of two things: anxiety in patients about how to handle an exacerbation, or failure to recognise deterioration in condition before a crisis occurs. It makes sense to enable patients to gain knowledge in a structured way to give them greater confidence about their diseases. Many people look up information anyway on the internet. We need to harness that natural inquiry and interest as part of the care system.
It is this element where technology can play a significant part. Imagine a situation where as a patient you can input your own recorded blood pressure (eliminating white coat syndrome) or blood sugar, or weight into an app. You can track your data in a time series graph and that graph is automatically available to your clinical provider. There can be automated responses if the readings are outside your personalised norm. This response might refer you to your pre-organised electronic care plan, and prompt your provider to call you. This is not the future, but exists now in 2013.
The key to facilitating co-management by patients is the availability of electronic and remote support. Less sophisticated versions of what is described above are features of many telehealth systems. These are remote monitoring systems where people input data which is reviewed at a central location. The best systems have two way communication and mobile platforms. Sadly many don’t. Many telehealth projects simply use the electronics as an add on to the existing method of delivery, rather than as a means of transforming the care model. For example, appointments might still be made in the same way, nurses might still visit in the same way with the same protocols, and he patient data duplicated by professionals or ignored in consultations. In short the investment is wasted. The mantra has to be: change the system first, put the kit in second. However, there is strong evidence that if technology is used to involve patients in their own care as part of a wider system change, there are reductions in unscheduled admissions, and even mortality. The whole system demonstrator project evaluated in England covered 6000 patients who used telehealth. The results showed a 20 per cent reduction in unscheduled admissions, and a 45 per cent reduction in mortality for some categories of patients. Much other literature also shows that empowered patients who co-manage their condition have better clinical control and outcomes. And this is not simply the better educated, higher income patients. Most people are interested in their own health, most can contribute to its management in some way, and increasing numbers have access to the internet via smart phones.
The rise in the number of people with multiple long-term conditions threatens to overwhelm most healthcare systems. Care based around individuals in the community, rather than hospital, is the only fiscally rational option—and produces better outcomes. A key shift in mindset is required for the most under used resource in healthcare to be utilised as part of the care system —the patients. Embracing technology catalyses that shift. Fears from professionals’ Patients don’t have the knowledge, ‘It is unsafe’, ‘It undermines my status’ are ungrounded in experience and often mask a vested, and sometimes economic, interest in status quo. But status quo is not an option, and the volume of demand is such that professional livelihoods would not be affected. The truth is that the digital revolution will come to healthcare, just as it has to other service industries. Patients will be able to seek the service they want from outside their national boundaries and the resistance of some professionals and organisations will be by-passed. Better, instead, to get ahead of the curve, and recognise the inevitable.