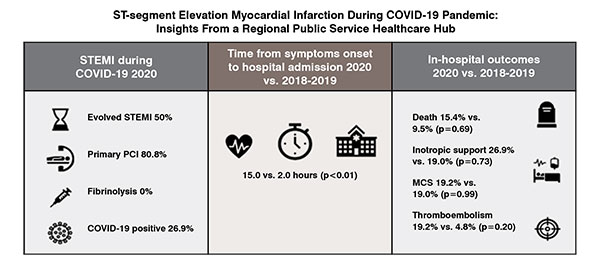
The COVID-19 pandemic may have profound indirect consequences on the epidemiology, phenotype, and management of acute cardiovascular diseases. Our study shows, in a cardiovascular regional public service healthcare Hub, during COVID-19 pandemic, a significantly longer time from symptoms onset to hospital admission among patients with acute myocardial infarction compared to the same period in the previous two years.
The coronavirus disease 2019 (COVID-19) pandemic has an enormous impact on social, economic, and healthcare networks. Every sector of the healthcare system has been hit by the pandemic and must now face significant worldwide re-arrangements on access to cure and clinical priorities, including among the others, re-organisations of cardiovascular health systems. In particular, the Emergency Medical System (EMS) has been reshaped across the globe to optimise the management of COVID-19 patients and at the same time continue to guarantee adequate care for patients with acute cardiovascular conditions.
Acute Coronary Syndromes (ACS) is the term used to define a range of cardiovascular conditions associated with a sudden reduction of blood flow (ischemia) to the heart muscle (myocardium). One of these most serious conditions is acute ST-segment Elevation Myocardial Infarction (STEMI). It is a frequent disease still associated with high mortality, mandating rapid management with reperfusion therapy, with the aim to promptly restore blood flow to the ischemic myocardium. Reperfusion therapies encompass primary percutaneous coronary interventions (PCI) and fibrinolytic therapy.
In the setting of STEMI, timely reperfusion therapy is crucial because a short ischemia time is associated with better clinical outcomes, lower short and long-term mortality. The impact of timing from the onset of symptoms to reperfusion as well as the creation of networks to supply around-the-clock fast access to primary PCI has definitely improved STEMI outcomes. Total delay from symptom onset to coronary reperfusion is both patient-dependent (delay from symptom onset to first medical contact) and healthcare systemdependent (delay from the first medical contact to coronary reperfusion). During COVID-19 pandemic both components were subject to increased delay.

We indeed showed that the delay from symptoms onset to hospital admission was at least 7-fold longer during COVID-19 outbreak compared to previous years, with a 50 per cent rate of late presentation (i.e., patients presenting > 12 hours from the onset of the symptoms). This observation has been confirmed by other studies suggesting larger delays in seeking medical assistance despite worrisome symptoms during the epidemic.
Explanation of this phenomenon may involve several factors. The fearrelated medical care avoidance may be associated with high tolls in terms of outcomes, in any medical setting. Fear can lead to an inappropriately high perceived risk related to hospital admission and medical evaluation. It can be a major determinant that makes patients reluctant to activate EMS. During epidemics, hospital avoidance behaviours have been reported and were traditionally associated with misconceptions about disease severity and transmission modes. For this reason, while the direct effect on deaths of COVID-19 has been substantial and obvious, concerns have also arisen about the indirect consequences of the pandemic. Hospitalisations for acute cardiovascular conditions have declined, suggesting that patients may be avoiding hospitals because of fear of contracting SARS-CoV-2. Our study somewhat confirms this observation: we, indeed, observed a lower-than-expected rate (as compared to previous years) of STEMI admissions to our Institute after the first Italian case of COVID-19 in Lombardy.
Moreover, failure to distinguish cardiac ischemia and COVID-19 related symptoms is possible. Sometimes there can be an overlap of respiratory symptoms with atypical ACS presentation that may confound patient perception and further delay proper EMS activation.
From a healthcare perspective, an attempt to contain SARS-CoV-2 outbreak should not mitigate the efforts spent in minimising total myocardial ischemia time. The COVID-19 pandemic placed the management of STEMI patients in a challenging situation due to the need to balance timely reperfusion therapy and maintaining strict infection control practices. For this reason, COVID-19 pandemic has led to a reshaping of the healthcare system to provide timely response and care to ACS patients. Re-organisation of the cardiovascular emergency network in Hub and Spoke hospital may reduce the unjustified exposure of individuals (i.e., patients in need of non-urgent procedures and their relatives) to the hospital and surrounding environment and affecting only marginally total ischemia time.
For instance, in the north of Italy, the Lombardy region was one of the first worldwide to be hit hard by SARSCoV-2 infection, apart from China. Under normal conditions, Lombardy has 55 cardiac catheterisation laboratories offering 24/7 service for ACS to approximately 10 million inhabitants. In order to continue to treat ACS patients according to current guidelines while preventing their exposure to SARS-CoV-2, the number of hospitals with catheterisation laboratories acting as Hubs has been reduced to 13, with the remaining hospitals working as Spokes.
Excess strain on health care systems, imposed by the COVID-19 outbreaks, may also play a detrimental role. Of note, the indirect health impact of a pandemic was already described during other pandemics. During 2014-2015 Ebola outbreak in Africa, healthcare systems were overwhelmed with a significant negative impact on diagnosing and treating the region's major endemic diseases: malaria, HIV/AIDS, and tuberculosis. The deaths caused by these diseases almost equaled the deaths caused by Ebola. During the 2009 influenza pandemic, an increase in mortality attributable to acute myocardial infarction and stroke was observed in the US. Similar phenomena may have also occurred during current COVID-19 pandemic. Indeed, in some regions of the United States, during the initial phase of the COVID-19 pandemic,there was an increase in deaths caused by ischemic heart disease and hypertensive diseases. A recent study based on an autopsy series of deaths during the pandemicfound that reduced access to health care systems (for conditions such as myocardial infarction) was further likely to be identified as a contributory factor to death, rather than undiagnosed COVID-19.
Treatment recommendations and guidelines may require a revision to minimise the SARS-CoV-2 spreading and prevent infection. European and American guidelines recommend primary PCI as the preferred reperfusion therapy, provided that total ischemia time is acceptable. However, during the COVID-19 pandemic, some expert claimed that PCI might be not the preferred reperfusion therapy. As mentioned above, the clinical benefit is mainly dependent on rapidly achieving first medical contact-to-reperfusion time within 90 to 120 minutes, and this may have been difficult to realise during the pandemic. In addition, isolation and infection control policies may increase the in-hospital delay when activating the catheterisation laboratory. Building on this, the Chinese Society of Cardiology has released a consensus statement: to cope with logistic issues and minimise healthcare workers exposure, fibrinolytic therapy is preferred over primary PCI for haemodynamically stable STEMI patients diagnosed with or suspected to have COVID-19 infection.
In some regions, healthcare systems were pushed to adapt and reallocate resources rapidly to care for the surge of patients with COVID-19.It has led to a bed shortage that might have hampered best care delivery to acute cardiovascular patients. Many cardiac intensive care units and cardiology wards have, indeed, been transformed in COVID-19 wards. In parallel, this may have led to delays in access to care or the delivery of suboptimal inpatient and procedural care for non–COVID-19 patients. The cancellation of outpatient cardiovascular visits has deferred access to medication prescriptions/refills and important diagnostic testing, which may have had direct detrimental consequences, especially in high-risk patients. In addition, the delay of semi-elective cardiovascular procedures (e.g., transcatheter aortic valve replacement) may have adversely affected patients with serious cardiovascular diseases with profound prognostic impact.
Finally, SARS-CoV-2 infection might also have had a possible direct pathogenetic contribution to cardiovascular events. Preliminary reports suggest an increased risk of cardiac complications among patients with COVID-19, including myocardial injury, myocarditis, ventricular arrhythmias, and cardiogenic shock, associated with a higher risk of mortality.
In summary, SARS-CoV-2 pandemic has profound consequences for cardiovascular diseases. Effects are both direct and indirect, leading In summary, SARS-CoV-2 pandemic has profound consequences for cardiovascular diseases. Effects are both direct and indirect, leading to a significant impact on patient management and prognosis. Besides direct factors, complex logistic, social, psychologic, and educational factors may impact the clinical picture and epidemiology of acute cardiovascular diseases.
There is a clear urgent need to improve public health messaging, communication, and education to ensure that patients with emergent conditions seek and receive proper medical care, particularly in regions currently experiencing surges or resurgences of COVID-19 cases. Patient education programmes can critically reduce total ischemic time by rising the awareness of ischemic symptoms and prompting immediate EMS contact. In this challenging scenario, telemedicine might provide an alternative avenue to provide medical education for STEMI patients and avoid unnecessary mortality. The medical community needs to balance the utmost efforts to limit the propagation of the COVID-19 pandemic with the imperative to prevent compromise in acute cardiovascular care.