
Capillary blood (fingerstick) sampling is increasingly being used worldwide due to the growing availability of point-of-care (POC) testing (Figure 1). With anaemia affecting approximately 25 per cent of the global population, and a high prevalence in developing countries, haemoglobin (Hb) is the most frequently performed test in POC haematology.1
POC haemoglobin testing can deliver accurate results in settings where a benchtop laboratory haematology analyser is not practical. Such locations include field settings where mobility and simplicity are essential, or resource-poor locations where dedicated laboratories are not available. Notably, pharmacies are increasingly offering Hb POCT in such situations.
However, Hb values are prone to being affected by pre-analytical errors, with incorrect capillary blood sampling being the most common reason leading to inaccurate POC haemoglobin results.2 Therefore, personnel drawing blood must adhere to strict and standardised blood sampling techniques to ensure accurate and consistent POCT results that are comparable to laboratory techniques.
For this reason, detailed capillary sampling guidelines have been published by both the Clinical and Laboratory Standards Institute and the World Health Organization.3,4 This article provides an overview of capillary sampling best practice.

It is important to understand the common causes of pre-analytical errors and reduce their impact on the haemoglobin result. Variability in reported haemoglobin values can be caused by a number of physiological factors,such as: gender, body position, dehydration, smoking, or altitude. As previously discussed, it can also be significantly affected by pre-analytical errors arising through incorrect capillary blood sampling technique.
Detailed below are some of the most common sources of error that healthcare workers should be aware of in order to appreciate the importance of adhering to standardised best practice capillary sampling procedures:
• Choice of lancet – This must make a sufficiently deep puncture to ensure an adequate flow of blood. 1.85 to 2.25mm is recommended for adults, depending on the thickness of the skin. For children aged below 8 years, the penetration depth should not exceed 1.5 mm.2
• Puncture site - Selecting the correct finger and puncture site will ensure best chance of good consistent blood flow and minimise pain for the patient. The middle or ring finger should be used, ideally of the non-dominant hand, as they are generally less calloused and less sensitive to pain compared to the index finger or thumb. The thumb should also be avoided due to its pulse (arterial presence). In the fifth finger the distance between the skin surface and the bone is too small.4
The puncture should be slightly off centre from the central, fleshy portion of the fingertip – near the side where the skin is thinner with fewer nerve endings and less pain sensation, but not on the very side of the finger.
• Cleaning, disinfection and drying - Cleaning and disinfection of the puncture site is essential to remove any potential contaminants that could affect the reading or jeopardise patient safety. The puncture site must also be dried completely, after cleaning, to remove any remnants of alcohol solution that will dilute the blood sample and cause false low readings.
• Applying too much pressure around the puncture site - The finger can be massaged gently before and after the puncture to stimulate blood circulation, but not going beyond the first knuckle. Maintaining a light pressure at the moment of puncture ensures effective penetration. However, the finger should not be pressed too hard as this will push fluid from the tissue into the blood and cause false low readings.
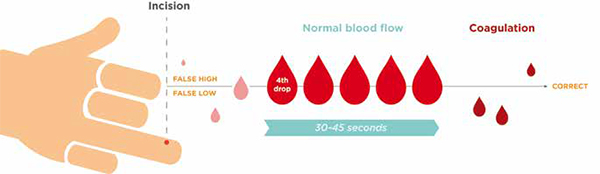
Another key factor that influences Hb measurement is capillary flow. Typically for haemoglobin, the first 1-3 drops after puncture show a higher degree of variability of the Hb concentration, independent of the analytical device used for the test. It is for this reason that these first few drops of blood should be wiped away.
The highest accuracy is generally reached from the 4th drop after puncture, with good capillary flow occurring for a period of 30-45 seconds. After this time, coagulation will occur where blood clotting would lead to inaccurate Hb results if blood is sampled then. Figure 2 demonstrates the ideal capillary blood sampling window.
The most important factor to reduce pre-analytical errors is the presence of a free spontaneous blood flow, especially as neither the size of the drop nor the time of collection following the puncture is well defined and manufacturers’ recommendations on this subject vary.
Best practice for capillary sampling can avoid the majority of pre-analytical errors.2 Therefore, in addition to following a standardised documented procedure, it is essential to ensure that all personnel taking blood samples are properly trained. Effective and continuous operator training and practice must be in place to eliminate pre-analytical errors and to obtain correct results for Hb testing, especially from capillary sampling.
In conclusion, with good operator training and best practice procedures in place, as well as physiological factors considered with the correct reference ranges applied, then Hb testing can be very reliably undertaken in a wide variety of POC settings.
References:
1. Briggs C et al, Where are we at with point- of- care testing in haematology? British Journal of Haematology, 2012, 158, 679–690
2. Massimo Daves et al, Evaluation of capillary haemoglobin determination for anaemia screening in blood donation settings Blood Transfus. 2016 Sep; 14(5): 387–390.
3. Ernst DJ, Balance LO, Calam RR, McCall R, Szamosi DI, Tyndall L. Procedures and Devices for the Collection of Diagnostic Capillary Blood Specimens. 6th ed. Approved Standard GP42-A6. Wayne, Pa: Clinical and Laboratory Standards Institute, 2008. Available at: https://clsi.org/standards/products/general-laboratory/documents/gp42/. Accessed July 6, 2017.
4. Dhingra N, Diepart M, Dziekan G, et al. “Capillary Sampling,” in WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy. Geneva, Switzerland: World Health Organization, 2010. Available at: www.ncbi.nlm.nih.gov/books/NBK138654. Accessed July 6, 2017.