
This article will include the evolution, the current state, the issues and challenges, and foresight into where Indian healthcare segment can be at the current pace and where it ideally should be 10 years down the line. It will also include how Health IT which includes HIS, SMAC, and virtual health (telemedicine) have been playing a role as an enabler and why the investment in these technologies by the provider segment is important in India.
Digitising healthcare is a vision aimed at making the world an even smaller place and bringing the patient closer to the provider, if not physically,virtually. Digital healthcare essentially circles around two main areas in healthcare: accessibility and affordability. This visionencompasses digitising all patient health records through an EMR or EHR, integrating the EMR with e-Prescription (prescription for medications reaching the pharmacy directly where the patient can go and collect it), PACS (archiving of radiology images electronically), etc., performing real-time data analytics based on the data captured and using the analysed data for clinical decision support or for predictive diagnosis and treatment of patients.
All of this is what providers do within the boundaries of the healthcare organisation. Outside the boundaries, use of mobile solutions and enabling of remote consulting and home care through virtual health or telemedicine is another segment that is allowing faster, more efficient, and more accurate care of patients. But even when most of us acknowledge these benefits and are moving in the direction of digitisation, then why is the transformation taking so long? Why are Indian providers’ mindsets still not acclimatising completely to this change? Why does the gap remain?
On 15th August, 2014, the new Prime Minister of India made a clarion call to move towards a digital India by revolutionising healthcare delivery using telemedicine. The models of tele-medicine and m-health, which initially began as proof-of-concept, have been proven to be scalable and replicable in other resource poor settings, highly effective in enhancing healthcare accessibility. However, the foundation of remote healthcare delivery lies in the increased adoption of the health IT (EHR/EMR) across Indian hospitals. The healthcare IT ecosystem still remains in the nascent phase, wherein integration of labs and pharmacies via the internet ensuring seamless communication with the clinicians still remains a recent development.
ICTsolutions for developing countries often require a different approach than that used in developed countries and organisational and user needs can be different due to cultural factors, such as overcoming paper-based systems, data-entry hassles, and resistance from doctors and hospitals towards a more transparent care scenarioor a lack of computing skills among staff all of which may complicate adoption. Large corporate hospitals in India still spend under
 1 per cent of their operating budget on IT, as compared to 3 per cent in the west and only 6 hospitals in India have reached the stage 6 Level on the EMR adoption model of the HIMSS. Overall, the scope of HIT services is restricted to metro and Tier I cities, and success is expected to depend on factors such as cost versus benefit comparison, along with clear and quicker ROI according to a recent report on Health IT in India.
1 per cent of their operating budget on IT, as compared to 3 per cent in the west and only 6 hospitals in India have reached the stage 6 Level on the EMR adoption model of the HIMSS. Overall, the scope of HIT services is restricted to metro and Tier I cities, and success is expected to depend on factors such as cost versus benefit comparison, along with clear and quicker ROI according to a recent report on Health IT in India.
Despite these restrictions, there is much reason to cheer as some Indian hospitals have undertaken crucial initiatives in the digital health space, which serve as benchmarks for the Indian healthcare industry in the years to come. Max Healthcare has been one of the first movers in the adoption of EHR, and was the first hospital in India and only sixth in Asia to achieve 'Stage 6' on the EMR adoption model from Healthcare Information and Management Systems Society (HIMSS) in 2012. This was engendered bythe implementation of an open source EHR solution (World VistA) with CPOE (Central Physician Order Entry), CDSS (Clinical Decision Support System) and BCMA (Barcode Medicine Administration) which ensured the documentation of the entire course of the patient’s stay in the hospitalby the integration of all transcripts, prescriptions and billing information into the system in order to provide analytical insights for improving health outcomes. The hospitals’ transition to the increased usage of data analytics to improve treatment regimens for many disease conditions was a first step towards moving from a traditional measurement of success of a healthcare facility by mere financial performance to clinical performance indices, which would be a representation of the overall health of their patients.
With such socio-technical approach towards overcoming technological and non-technological barriers, Max Healthcare was able to provide real time access to patient records using the EHR by maintaining the continuity of the patients’ medical records and thereby reducing delays in clinical decisions. The enhanced clinical decision support systems enabled them to optimize manpower utilisation, particularly in tracking patient outcomes for better disease management such being the case with the prevention of hospital acquired Venous Thromboembolism and in analysis of health outcomes for various treatment modalities for breast carcinoma.
Apollo Hospitals, which has been the forerunner of integrated healthcare, has also contributed highly towards India’s digital health journey. During 2013-14, four Hospitals within the Apollo group achieved Stage 6 on the Electronic Medical Record Adoption Model (EMRAM). Apart from adopting international clinical standards, Apollo Hospital Group also creates population-specific clinical rules from population studies. In addition, unit drug dispensing dosage and excellent clinical decision support are present. As early as 1999, the Apollo Hospital Group (Apollo Telemedicine Networking Foundation) decided to extend its outreach and initiated the process of providing healthcare to suburban and rural India by adopting Information and Communication Technology for the telemedicine platform. Today, they run the oldest and largest multi-specialty telemedicine network in South Asia, which specialises in remote consultation and second opinion to both patients and doctors, improving access to quality healthcare due to distance and high costs. ATNF’s flagship web-enabled Telemedicine application 'MedintegraWEB’ enables doctors, nursing homes and hospitals to reach out to patients in inaccessible areas and provide interactive healthcare using modern telecommunication technology by collecting and converting the patient’s data into a secure and confidential Electronic Medical Record (EMR). Based on the investigation, the specialist offers his/her opinion which is transmitted back to the grass root (peripheral) where the doctor is able to treat the patient accurately and without any further delay.
ATNF has also been instrumental in demonstrating that 3G technology can be used in transferring health information, thereby, leading the m-health initiatives in India. Text, audio, and video data have been transmitted on a real-time basis and have facilitated interaction between the consultants at the Apollo Hospitals, Chennai and patients in the villages at the remote end. Using 3G, doctors at the tertiary hospital have been able to clinically 'examine' the patients through a high-quality web cam.
Growth in data, digitisation trends in health information and EMRs, improvements in collaborative data exchange, workflows and mobility, and need for better financial management have been recognised as the changing needs of the hospital enterprise. Additionally, patient demographic changes and chronic disease growth, cost control considerations, and importance of patient safety, have all come together to heighten the demand for Health Information Technology (HIT) in India, generating a potential US$1.45 billion health IT market by 2018. The main expectations of hospitals in future are linked to complete integration of systems, more shareable information platforms, and standardisation that could lead to user-friendliness, and access to mobile devices such as tablets, as well as advanced tools uptake like telemedicine and virtual meeting systems for knowledge sharing.
A contributing factor is that healthcare organisations are complex and include a variety of work practices. This includes strong interdependency of roles, and a hierarchy of distributed responsibilities. This interdependence can make imposing changes difficult because a small change in one person’s workflow may affect the performance of someone else’s workflow. Medical Informatics Systems (MIS) for such hospitals can thus be challenging to design and implement, and nearly half of them fail due to user and staff resistance. The increase in adoption of electronic health records, mHealth, telemedicine, and web-based services has made electronic patient data expand, necessitating the implementation of robust IT systems in Indian healthcare institutions.

 Challenges
ChallengesHospitals have noted that ease of integration with existing solutions is the main criterion they seek from Electronic Medical Record (EMR) vendors which brings us to our next discussion on this topic - the major challenges associated with implementation and successful adoption of health informatics solutions in India:
The transformational journey of 'Putting patient at the centre of care'
has begun but providers in India today still haven't been able to realise this dream in its true sense yet. It seems providers generally do not look at investing in health informatics as a long-term gain to improve operational efficiency and patient health outcomes; to them, it seems to come across as an expense from their budget to make themselves appear more competitive. One of the reasons is that users /clinicians at these hospitals have had a difficult time adapting to the technology and some of them still prefer pen and paper which again ends up getting filed in a drawer as opposed to a digital clinical note that gets saved on a secure server and is immediately available for review the next time the same patient shows up. Now, why would the user have difficulty adapting to a process that essentially is being imitated electronically? There have been cases where processes and workflows in hospitals are not followed to the 'T' and thus, when entering the entire mandatory information becomes a requirement, the users tend to resist because of the volume of data entry that may now be required which brings us to our next challenge.
One of the reasons for the technology not being able to provide its expected ROI to Indian hospitals is the lack of awareness among users/clinicians on how to 'optimally' use the technology to see maximum benefits from its use. This idea also ties back to the point made above on adoption. Users will adopt the technology better if they are well aware of how it will help serve the provider's goals and objectives with optimal use.
Think about it–a software product may be capable of doing the right analysis and generating the right reports but the results may be skewed or not accurate because the data entry (the first step in the process) itself may not be accurate or complete to allow generating valid results.
When providers in India implement a health informatics solution, the general expectation is to start reaping immediate benefits from the use. The thought process that ideally needs to be adopted by providers in India is to create an IT Strategy for the health informatics solutions to be deployed and outline the quick wins (initiatives that provide high medical value and require relatively lower fund requirement and time for implementation) and long-term milestones clearly and build KPIs to measure the achievement as time progresses to ensure the expected benefits are being realised at the expected point in time on the strategy roadmap.
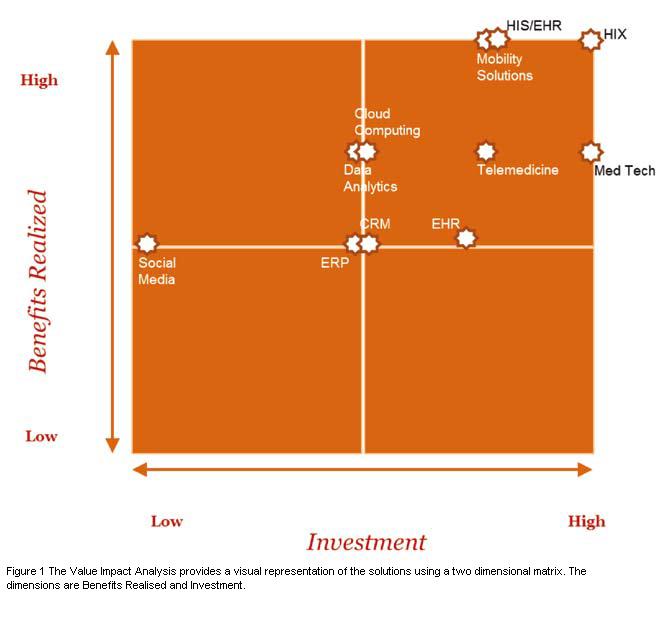
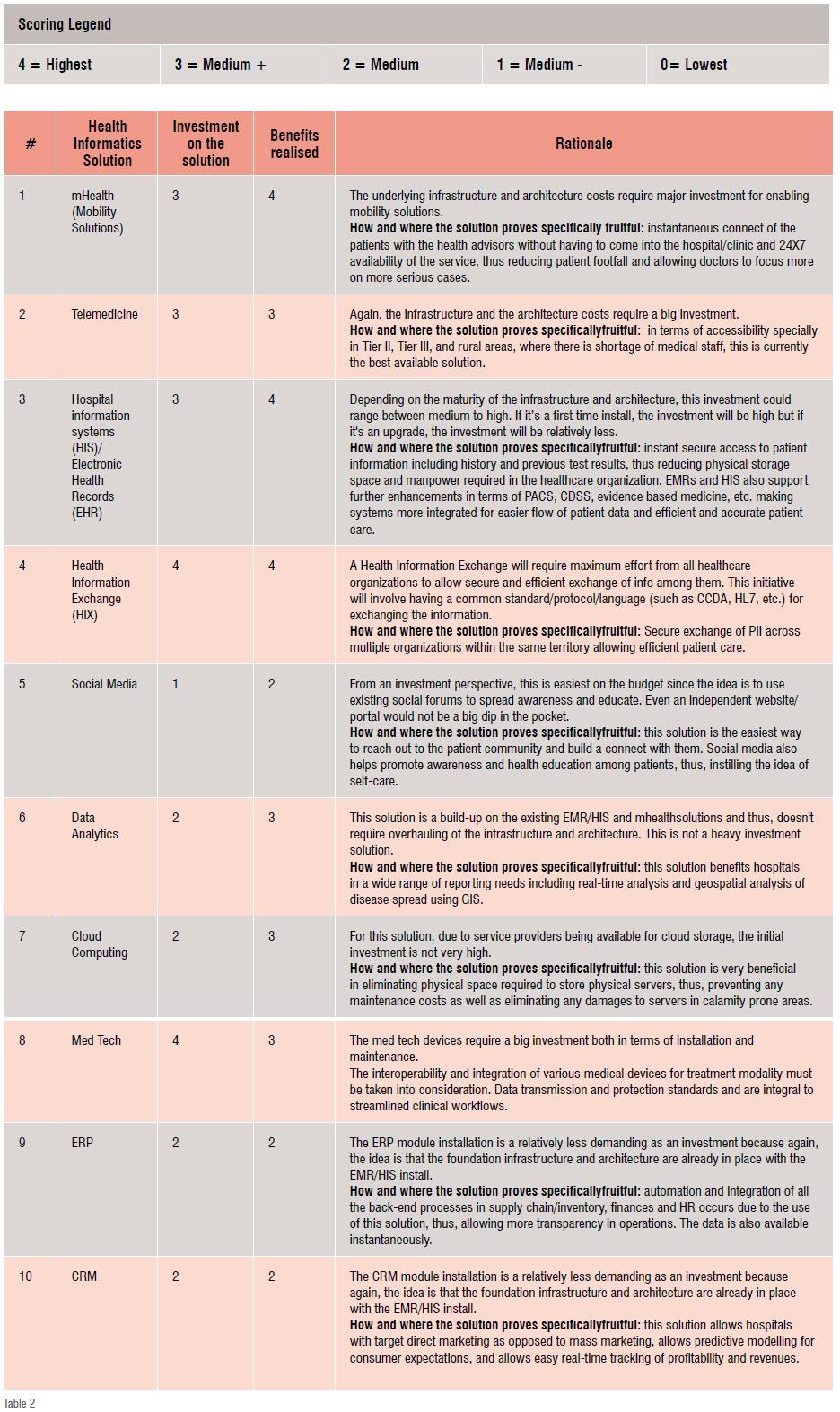
Having discussed these challenges, it would also help to understand the optimal use of the health informatics solutions considered by most healthcare organisations. In order to ensure providers pick the right solution to address their operational issues, the following is a breakdown of the solutions in terms of the investment made versus the benefits realised.
1. Max Healthcare’s EHR Journey: From Implementation to Data Analytics; Dr Sandeep Budhiraja; DrVibha Jain; Hardeep Singh; Official Journal of Indian Association for Medical Informatics (IAMI)
2. A case study of an EMR system at a large hospital in India: Challenges and strategies for successful adoption; Jeremiah Scholl, Shabbir Syed-Abdul, LuaiAwad Ahmed
3. Health IT in Indian Healthcare System: A New Initiative Sharma Kalpa; Research Journal of Recent Sciences
4. Healthcare Information Technology Market Outlook in India, Frost & Sullivan
5. Apollo Telemedicine Networking Foundation (ATNF) Case Study: ACCESS Health International and Results for Development Institute / Rockefeller Foundation