The plague pandemics have devastated the world through the centuries, remaining etched in history as scourges that have involved a large part of the population with high mortality rates, from the Justinian plague (541 AD) to the terrible black death (334), originated in China and spread along the great trade routes to Constantinople and then to Europe with a mortality of 60 per cent, to the modern plague of 1860.
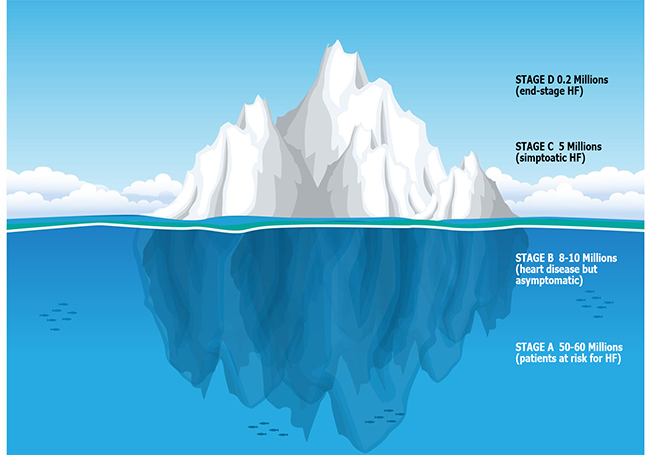
In this century, despite steady progress in terms of prevention and therapy, Heart Failure (HF) is reaching such a spread that it can be defined as a pandemic disease, just like a plague. HF is a major public health problem, with a prevalence of more than 5.2 million in the United States and more than 26 million worldwide. Incidence and prevalence reported in the medical literature vary widely, mainly because different sets of diagnostic criteria have been used. Contemporary studies estimate the overall prevalence of HF in the US population to be about 2per cent-3 [1] However, these data represent just the tip of the iceberg; in fact, in US, including also patients in stages A (patients at high risk to develop symptoms and signs of HF such as with hypertension, diabetes, coronary artery disease, family history of cardiomyopathy) and B (patients with structural heart diseases but asymptomatic), the numbers of HF dramatically rise from 5.2 million to 63.2-75.2 million, leaving as normal only a third of the entire US population [2] (Fig. 1). The incidence is 600.000 new HF cases per year in Europe and 500.000 in the USA with 1 in 5 adults over 40 years will have HF in their lifetime and 1 in 5 HF patients will die within 1 year. The patients suffering from HF have 6-9 fold increase in sudden death risk. The 3 major risk factors are age, diabetes and obesity. The prevalence of HF will increase from 2.8per cent (2010) to 3.5per cent (2030) in the USA with an increase of health system costs from US$24.7 billion (2010) to US$77.7 billion (2030). [3-5]. Heart failure inflicts both direct costs to healthcare systems and indirect costs to society through morbidity, unpaid care costs, premature mortality and lost productivity. The global economic burden of HF is very high. The overall cost of heart failure in 2012, in both direct and indirect terms, across the globe, has been evaluated [4]. Countries were categorized according to their level of economic development to investigate global patterns of spending; 197 countries were included in that analysis, covering 98.7per cent of the world's population. The overall economic cost of HF in 2012 was estimated at US$108 billion per annum. Direct costs accounted for ~60 per cent (US$65 billion) and indirect costs accounted for ~40per cent (US$43 billion) of the overall spend. Heart failure spending varied widely between high-income and middle and low-income countries. High-income countries spend a greater proportion of direct costs: a pattern reversed for middle and low-income countries. Japan and South Korea spent 553,393 and 81,422 millions of dollars for HF in 2012, respectively.
Hospitalisation comprised approximately 80per cent of direct treatment costs for heart failure [5]. In an analysis of 1.1 million Medicare patients in 2010, hospitalisation costs for heart failure were US$91.9 million, accounting for 3.1per cent of the total expenditure. [6] The use of healthcare resources is predicted to rise over the coming decades as the number of patients with heart failure increases. Hospitalisations for heart failure in the UK are projected to rise by 50per cent over the next 25 years, [7] while the costs of heart failure treatment in the USA are predicted to more than double by 2030 [5].
Patients with HF who died within 1 year after an index HF encounter incurred markedly higher costs within 1 year (despite the much shorter post-index period) than those who survived, with the majority of costs attributable to hospitalisations for both patient cohorts. [8]
Rehospitalisation is common among patients with heart failure following their initial discharge, accounting for about 30per cent of all cases [9]. In European studies, reported rehospitalisation rates range from 24per cent at 12 weeks40 to 44per cent at 1 year after discharge [10]. In the USA, 30-day readmission rates were about 20–25per cent, however, readmission rates of 60–67per cent have been reported with longer follow-up [11] . Short-term survival is also poor, with 1-year death rates typically between 20per cent and 40per cent. Some improvements in short-term and in-hospital death rates have been observed in recent years. [12-14].
In an analysis of over 6.5 million heart failure hospitalisations in the USA, the unadjusted in-hospital death rate fell from 8.5per cent in 1993 to 4.3per cent in 2006, and the 30-day death rate decreased from 12.8per cent to 10.7per cent over the same period. [14] Another Medicare analysis also reported a decreased in-hospital death rate, from 5.1per cent in 2001 to 4.2per cent in 2005, although 180-day and 1-year all-cause death rates remained fairly constant at approximately 26per cent and 37per cent, respectively. [13] A reduction in the 1-year death rate from 31.7per cent in 1999 to 29.6per cent in 2008 was reported in an analysis of data from 55 million Medicare patients [12].
Despite some ongoing improvement, long-term survival of patients after an episode of acute heart failure also remains poor, with reported 5-year death rates of around 70per cent [15-17]. In a community-based study in the USA, the 5-year death rate improved from 57per cent for patients newly diagnosed with heart failure in 1979–1984 to 48per cent for those diagnosed in 1996–2000. [17]
Meta-analysis Global Group in Chronic Heart Failure (MAGGIC) [18] compared Survival in patients with HF-preserved EF with that in patients with HF-Reduced EF in a meta-analysis using individual patient data. Preserved EF was defined as an EF ? 50per cent. The 31 studies included 41972 patients: 10347 with HF-PEF and 31625 with HF-REF. Patients with HF-PEF had lower risk of death than patients with HF-REF, and this difference is seen regardless of age, gender, and aetiology of HF.
For patients, the physical limitations brought about by shortness of breath, loss of energy and fatigue associated with heart failure affect work, social and leisure activities. [19] Patients commonly experience social isolation, reporting limited ability to travel, socialize or take part in recreational activities. [20]
Psychological effects, including fear, anxiety and depression, are common among individuals with heart failure. [19] Furthermore, heart failure can have a marked effect on personal relationships, with the increasing reliance on others leading to feelings of guilt and frustration. In addition, family members often feel the burden of caring for a patient with heart failure, and these demands can have physical, emotional and financial effects on them. [19,20] Three different components make up patient self-care: maintenance, monitoring and management. Maintenance involves adherence to medication and lifestyle changes, while monitoring of the signs and symptoms of heart failure includes activities such as daily weighing to assess fluid retention. Self-care management means responding appropriately to any changes in symptoms – for example, by increasing the dose of medications prescribed for use as needed.
In conclusion, a lot of road has been covered, but otherwise it must be covered to try reducing the burden of this new plague. We should invest a lot of resources in preventing the transition from stage A to the other stages in order to avoid a further increase in the incidence of HF; we should move the management of HF out of the hospitals, with a home-care system employing disease-oriented care-givers or in territorial outpatient clinics, reserving hospitalisation only for the worst cases (stage C2-D). We should build risk models that identify the patients most predisposed to re-hospitalisation so as to be able to intervene to reduce the rate of re-hospitalisation of these categories. Only by implementing these health policies for HF control and management, we will avoid the noteworthy burden of HF not only in terms of mortality, but also in psychological, social and economic terms.
References
1. Lloyd-Jones D, Adams RJ, Brown TM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:e46-e215
2. Ammar KA, Jacobsen SJ, Mahoney DW, Kors JA, Redfield MM, Burnett JC Jr, Rodeheffer RJ. Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation. 2007 Mar 27;115(12):1563-70
3. Heidenreich PA, Trogdon JG, Khavjou OA, et al; American Heart Association Ad-vocacy Coordinating Committee, Stroke Council, Council on Cardiovascular Radiology and Intervention, Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular Nursing, Council on the Kidney in Cardiovascular Disease, Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933-944.
4. Cook C, Cole G, Asaria P, Jabbour R, Francis DP. The annual global economic burden of heart failure. Int J Cardiol. 2014 Feb 15;171(3):368-76
5. Heidenreich PA, Albert NM, Allen LA et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013;6:606–19.
6. Joynt KE, Gawande AA, Orav EJ, Jha AK. The Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA 2013;309:2572–8.
7. National Institute for Clinical Excellence. Chronic heart failure: management of chronic heart failure in adults in primary and secondary care. NICE clinical guideline 108. 2010: guidance.nice. org.uk/cg108/ (Accessed 21 October 2013).
8. Obi EN, Swindle JP, Turner SJ, Russo PA, Altan A. Healthcare Costs Among Patients with Heart Failure: A Comparison of Costs between Matched Decedent and Survivor Cohorts. Adv Ther. 2017 Jan;34(1):261-276
9. Cleland JG, Swedberg K, Follath F et al. The EuroHeart Failure survey programme – a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J 2003;24:442–63
10. Maggioni AP, Dahlstrom U, Filippatos G et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail 2013;15:808–17.
11. Kociol RD, Hammill BG, Fonarow GC et al. Generalizability and longitudinal outcomes of a national heart failure clinical registry: Comparison of Acute Decompensated Heart Failure National Registry (ADHERE) and non-ADHERE Medicare beneficiaries. Am Heart J 2010;160:885–92.
12. Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalisation and mortality rates for Medicare beneficiaries, 1998–2008. JAMA 2011;306: 1669–78.
13. Curtis LH, Greiner MA, Hammill BG et al. Early and long-term outcomes of heart failure in elderly persons, 2001–2005. Arch Intern Med 2008;168:2481–8.
14. Bueno H, Ross JS, Wang Y et al. Trends in-length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA 2010;303:2141–7.
15. Cleland J, Dargie H, Hardman S, McDonagh T, Mitchell P. National Heart Failure Audit: April 2011–March 2012. London: National Institute for Cardiovascular Outcomes Research, 2012.
16. Joffe SW, Webster K, McManus DD et al. Improved survival after heart failure: a community-based perspective. J Am Heart Assoc 2013;2:e000053.
17. Roger VL, Weston SA, Redfield MM et al. Trends in heart failure incidence and survival in a community-based population. JAMA 2004;292:344–50.
18. Meta-analysis Global Group in Chronic Heart Failure (MAGGIC).. The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012 Jul;33(14):1750-7
19. Thomas JR, Clark AM. Women with heart failure are at high psychosocial risk: a systematic review of how sex and gender influence heart failure self-care. Cardiol Res Pract 2011;2011:918973.
20. Jeon YH, Kraus SG, Jowsey T, Glasgow NJ. The experience of living with chronic heart failure: a narrative review of qualitative studies. BMC Health Serv Res 2010;10:77.