Background
Although India’s healthcare system has gradually improved over the past few decades, there still remains scope to bring it at par with neighbouring countries which have a better healthcare system in terms of accessibility, affordability and quality. The poor state of healthcare in India is attributed to the heavy burden of patients, lack of medicines and equipment and not so enough of government funding of healthcare initiatives, leading to high out of pocket expenditure. As recommended by World Health Organization (WHO)(1) the accepted norm for public spending on healthcare is 2.5-5.0 per cent of GDP, whereas India’s public healthcare funding remains at 1.2 per cent of GDP in the year 2017-18. In fact the National Health Policy, 2017 of India has one of its objective to enhance health expenditure by government to 2.5 percentage of GDP by 2025.
However, there is yet another aspect which needs to be further investigated. There are many low income countries, such as Bangladesh, that have lower Infant Mortality Rates (IMR) than India does, despite their lower public spending on healthcare, which indicates that it’s not merely the number which matters. Government healthcare spending in India could be more effective if larger fund allocation for healthcare are supplemented with effective and innovative interventions which aim to accomplish global standards specifically in rural and inaccessible areas.
Rural Healthcare system in India
An astounding 70 per cent or nearly two-thirds of the population in India still resides in rural areas and has no access or limited access to hospitals or clinics. Around 80 per cent of specialists serve in urban areas.The national norms for a three level rural primary healthcare system (Figure 1) consisting of the Sub-Centre (SC), Primary Health Centre (PHC) and the Community Health Centre (CHC) had evolved during the Sixth Five Year Plan and as a result, major expansion of rural healthcare infrastructure was seen during the Sixth and the Seventh Plans.The Eighth Plan focused on strengthening existing healthcare infrastructure to better the quality and the outreach services and the Ninth Plan improved upon the availability of primary healthcare facilities.
Inspite of a continual increase in the number of medical institutions in the country, there still remains a severe shortage of sub-centers, primary health centers, and community health centers.
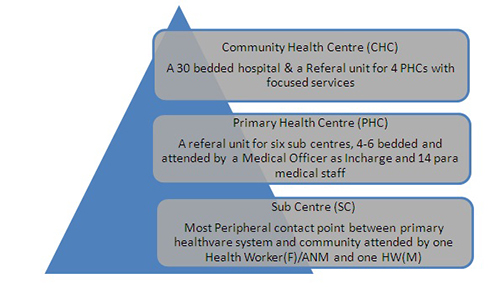
Figure 1: Structure of Rural Healthcare system
National Rural Health Mission under the Umbrella of National Health Mission (NHM):
The issues of infrastructure, human resources and inadequate public investment in healthcare are some of the governing factors for the present unsatisfactory performance of the Indian Public Health System. As a solution, the planners came up with a comprehensive mission oriented approach to revamp the rural healthcare delivery system called National Rural Health Mission (NRHM) in 2005 aiming to provide accessible, affordable, effective, accountable and reliable healthcare to all citizens and in particular to the more poor and vulnerable portions of the population.This was in accordance with the outcomes envisioned in the Millennium Development Goals (MDGs) of the United Nations as well.
Provision of the Mobile Medical Unit (MMU) in every district across the country was one of the key strategies employed to strengthen healthcare facilities and take healthcare to the doorstep of the public in rural areas. The states were, however, expected to ensure the adoption of the most suitable and sustainable model of MMU based on their local requirements.
Under NHM alone, about 1107 MMUs in 333 districts are being run in order to deliver healthcare services to difficult areas besides the Emergency Response Vehicles and ambulances for referral transport services in eighteen states of our country(2). These MMUs were related to select reproductive and child health services and to the national disease control programmes and not to the wider range of healthcare services that were needed. Besides Government initiatives, there is a good variety of MMUs currently being implemented by charitable organizations or NGOs too.
The Concept of Mobile Medical Units
Despite notable gains in coverage, specifically when India is moving ahead towards achieving Universal Health Coverage, reaching populations in the most remoteareas remains a constant challenge. Rural areas are characterized by low population density, which implies relatively great distances between people. This geographical fact itself multiplies the barriers to healthcare services many fold. In addition to the distance problem, one witnesses the lack of healthcare manpower in rural areas, a factor that cannot be fixed with money. So, even though we recognise a great need for healthcare in rural areas, simply pouring money into these regions is not the complete answer. Therefore, a system of medical care needs to be implemented large scale which can efficiently produce a positive effect within the available resources. Lack of services through fixed structures is a crucial issue that should be addressed as a matter of priority. MMUs can be a key service strategy to reach the vulnerable and marginalised populations living in remote, difficult areas as well as for communities that are cut off from mainstream services on account of climatic conditions and geography. Not to mention that they have played a significant role in the delivery of health services to uninsured or under insured populations.
Even though the concept of mobile hospital is much older than our imagination, there is less well documented (limited published literature) in the field. Past literature on this topic remains largely anecdotal, patchy and atheoretical. A mobile health service is any form of medical care in which services are brought to the patient rather than having the patient travel to the services. It can be as simple as a medically-trained person bringing his talent to the patient's bedroom as opposed to a 50-feet container with lacs of rupees worth of machinery manned by an entire medical team.
Mobile health units can be classified according to the presence or absence of mobile equipment. Travelling medical personnel carrying only small amounts of supplies are called mobile teams. Mobile services including equipment in addition to personnel are known as mobile facilities. When speaking in general of mobile personnel, facilities, or both, the term mobile unit is used. Simple mobile units can be jeeps or cars for the transport of personnel with basic equipment and drugs. Ambulances with oxygen, stretchers, splints and bandages are a form of mobile unit. A more complex mobile unit may contain a sink with running water, cabinets, a generator for electricity, refrigerator, examining table, simple laboratory facilities such as a microscope or centrifuge, x-ray equipment, dental equipment, and so forth. Of course, as the unit becomes larger, its mobility decreases, especially on the muddy narrow roads of many underdeveloped countries or hilly terrain. Different types of mobile units also have different purposes. Some are designed to provide comprehensive primary care to people who have no access to stationary facilities. Others cater to some specific aspect of health and provide for more specialized care e.g. bone density check up, ophthalmic units for eye care, immunization, dental checkups, cardiac units for coronary care, Cancer screening or multiphase screening etc.
There are multiple factors which need to be considered and examined when deciding whether to bring health services to the patient rather than requiring the patient to travel to the services. Firstly, the geographic-demographic facts must be taken into consideration, and these may lead one to the conclusion that mobile units are necessary for any utilization of health services to take place, or that mobile units are at least one feasible way of providing services. Second, one must determine whether the type of health service desired is compatible with the innate qualities of mobile units, i.e., periodicity, simple facilities, mobility and usually simply-trained personnel. Finally, if on the basis of these considerations, mobile units are a reasonable answer to the health delivery problem, a cost-benefit study should be done to determine whether a mobile system has a higher benefit-to-cost ratio than a system of fixed services.
Conclusions and Recommendations
Though mobile units have great potential in rural areas, especially in certain aspects of preventive medicine and emergency care, the concept of MMUs must not be embraced without a thoughtful analysis. Pre-launch studies for assessing the needs of that particular area or studying the disease profile are essential for successful implementation and long term sustainability of the intervention. An assessment of patient satisfaction by seeking feedback after regular intervals is mandatory from users. In fact, understanding the reasons for non-utilization is also important to improvise and to get a sufficient framework for policy analysis.
The most important disadvantage of mobile units is the lack of continuous care for patients by medical personnel. Therefore, it cannot replace the permanent structures. A suitable mix between the stationary and the mobile policy can fine-tune the healthcare system to the particular needs of a concrete country. It may be preferable to supplement the stationary hospitals or healthcare stations by some few mobile units providing care even at a rather low level instead of excluding large parts of the population totally from medical supply. There does not seem to be a unanimous agreement upon telemedicine. Under such an environment, it would be advisable for stakeholders involved to know the limitations of this technology and work out strategy as appropriate to their environment. More studies need to be conducted, preferably in a prospective manner based on scientific parameters by investigators drawn from diverse background to avoid bias.
The public-private collaboration will continue to engage policy attention and is justified on the basis of resource limitations for expansion to meet the growing demand. There is little evidence to suggest the institutional capacity of the government agencies to design, negotiate, implement and monitor such partnerships, scope and coverage of the services for potential partnerships with the private sector. Detailed studies are therefore required to get an insight of the kind of partnerships and linking them with the results targeted.
At this point of time, when the network of MMUs has been implemented in almost the whole of India, it becomes very important to take up research studies to analyse the impact of these MMUs. We need to understand whether the launching of these MMUs can really play a pivotal role in providing healthcare services to the unreached people of rural India.Thorough studies aiming to assess the impact are therefore required to be undertaken to get a ample framework for policy analysis.
1. WHO Discussion Paper (How Much Should Countries Spend on Health?) Available from: http://www.who.int/health_financing/en/how_much_should_dp_03_2.pdf
2. Ministry of Health and Family Welfare, Annual Report 2015-16, Department of Health and Family Welfare, Government of India.