
Medical gases and vacuum systems are used in hospitals to provide safe and cost-effective source of medical gases for the clinical applications. In this article, medical gases are described in terms of types and purposes. Moreover, a general overview of Medical Gases Pipeline Systems (MGPS) components and design is covered.
Overview
Medical gases are used for patient's healthcare in different ways. In the early of 1950s, healthcare providers recognised the hazards of using heavy high pressure cylinders of medical gases. Instead, medical gases and vacuum systems are provided by medical gases pipeline system (MGPS). It is safe, permanent and cost-effective mean of provision. In general, medical gases are specific gases that are separated from the air individually for various medical applications. Commonly used medical gases in hospitals are
• Oxygen (O2)
• Nitrous oxide (N2O)
• Medical air 400 KPa or 4 bar (MA 4)
• Medical air 700 KPa or 7 bar (MA 7)
• Carbon dioxide (CO2)
• Nitrogen (N2)
• Medical vacuum
1. Oxygen (O2)
Oxygen is the most important gas on the earth; it formed about 21 per cent of the natural air. In application, it is used as a medical gas to sustain life. Moreover, it is used to drive anesthesia machines and ventilators in addition to other methods for manual ventilation. Three sources are used for oxygen supply; vacuum-insulated evaporator (VIE) or bulk tank, cylinders, and oxygen concentrator (PSA) system. Further, oxygen is coded in white color.
2. Nitrous oxide (N2o)
Nitrous oxide is a medical gas administrated via anesthesia machine. It is mixed with oxygen and various anesthetic agents. Therefore, operating rooms are sole location of nitrous oxide. Usually a manifold supply system is the source of nitrous oxide gas. Cylinders are coded with blue color as well as the pipelines.
3. Medical air 4 bar
In general, medical air 4 is used for respiratory applications. The source of supply can be a medical gas manifold system or a medical compressor system. The color code is black color.
4. Medical air 7bar
Medical air 7 is known as surgical air because it is used mainly to derive some surgical equipment such as tourniquet and bone saw. The supply source is similar to medical air 4.
5. Carbone dioxide (CO2)
Carbone dioxide is a medical gas used for insufflations purpose in open heart surgery and laparoscopy procedures. Usually portable cylinders are the source of CO2 which are coded with grey color.
6. Nitrogen N2
Nitrogen for surgical power tools is likely to be used only on the sites where it is available for the production of synthetic air.
7. Medical vacuum
Medical vacuum is provided by means of a vacuum central plant. The vacuum system should always be used in conjunction with vacuum control units that include vacuum jars. In fact, it is not a gas, it is a negative pressure used for suctioning patients and for anesthetic gas scavenging system. Typically, vacuum is delivered at pressure of 400 mmHg (53 KPa) below atmospheric pressure. Vacuum pipes are known with its yellow color.
A. System components
Each medical gas must be supplied from a separate system. It is essential that all parts of each system are gas specific to ensure that there is no possibility of cross-connection between systems. Indeed, a common configuration is designed to each system as shown in Fig.1 including the following components.
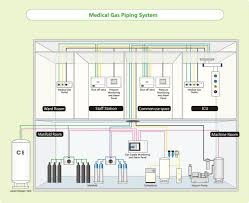
Fig. 1 Medical gas piping system configuration
1. Sources
Sources are supplies that produce the flow of medical gases through piping networks. There are four main sources for medical gases:
Bulky systems
It consists of special insulated vessels, vaporizers, and regulators. Theses systems can be constructed with cryogenic vessels or a high-pressure manifold, depending on the usage. Typically, oxygen, nitrous oxide, and carbon dioxide are supplied to large hospitals in cryogenic tanks.
Manifold systems
It consists of high pressure cylinders on 2 banks; one is a back-up to the other. In addition, main control panel is installed for primary and secondary regulators, pressure regulators, and warning lamps. Figure 2 presents an example of manifold systems for nitrous oxide.
Medical air treatment systems
Medical air treatment systems are usually 2 or more compressors equipped with a receiver, derivers, regulators, filters, dew point monitors, and carbon monoxide alarms. Produced air should be free of dust and moisture.

Fig. 2 An example of Nitrous oxide manifold system
Vacuum pumps
Vacuum pumps are mechanised devices that create a negative pressure in the piping system. The pumps should alternate automatically. A reservoir tank is used for storage to permit cycling on and off instead of continuous operation. Each pump should be capable of maintaining 75 per cent of calculated demand during peak time.
2. Piping networks
Medical gases and vacuum are distributed via the pipeline distribution system to provide gas or vacuum at the end-point or terminal units. The terminal units may be either wall-mounted or pendant-mounted. The pipes should be made of high quality copper, seamless type, and non-arsenic. Moreover, it should be protected against physical damage and corrosion and color coded as per gas content.
3. Valves
There are 2 types of valves; zone valves and service valves. Zone valves are used to isolate large parts of the system, i.e. rooms for modification and/or repair. In addition, zone valves are placed on corridor walls and should be labeled to indicate the rooms that they control. On the other hand, service valves are used to isolate certain part of the system for modification and/or repair. Accordingly, they are accessible by the clinical staff.
4. Warning and alarm systems
The function of warning and alarm systems is to give information for the responsible staff about the whole plant in case of failure detection or change requirement. This includes the sources, the pipes, the valves, etc. Therefore, there are 2 main alarm systems; master alarms and area alarms. Master alarm monitors the main gas lines and sources conditions. Area alarms are found on alarm panels and their function is to monitor the conditions of specific critical care area. According to NFPA standards, both master and area alarms must be reviewed and checked regularly.
5. Outlets and inlets
Outlets are points at which connections can be made to the medical gas piping system to supply gases under pressure, while inlets are supply vacuum. There are 2 styles of connections; quick connect and twist-on. Outlets should be gas-specific and also color coded as per gas content as shown in Fig. 3.

Fig. 3 A set of medical gases outlets/inlets
6. Secondary equipment
While hoses, gas flow meters, gauges, and vacuum regulators are not part of the pipeline system, they can contribute substantially to gas and vacuum consumption. These items should be checked regularly as a part of routine inspection procedures.
B. Design principles
In designing medical gases and vacuum systems, the goal is to provide a safe and sufficient flow at required pressures to the points of delivery (outlets/inlets). Moreover, these systems must meet specific requirements of served hospitals. The design should be carried out according to known standards such as NFPA 55 and NFPA 99. General information is required in order to design MGPS as follow:
1. Analyse each area of the hospital to determine next items:
a) Which piped-gas systems are required?
b) How many of each different type of medical gas outlet/inlet terminals is required?
c) Where should be location of outlet/inlet terminal?
d) Which type of and style of outlet/inlet terminal best meet the needs of the medical staff?
2. Anticipate any building expansion and plan in which direction the expansion will take place (horizontally or vertically).
3. Determine locations for the various medical gases supply sources.
4. Prepare the schematic piping layout locating zone valves, area valves, master alarms, and area alarms.
5. Locate station inlets and outlets at an appropriate height to prevent physical damage to attached equipment and accessories.
6. Medical gases and vacuum systems serving patients shall be independent of all other vacuum and gases systems serving laboratories, workshops, and research areas.
7. Design Medical gases and vacuum systems to deliver the following nominal pressures at the points of use: all pressure systems, except nitrogen shall be 50 psi (3.4 bar) to 55 psi (3.8 bar) at maximum flow; Nitrogen shall be 160 psi (11 bar) to 185 psi (12.7 bar) at maximum flow; vacuum shall be 15 to 19 inches Hg at most distant inlets.
8. Include anesthetic gas scavenging disposal system (AGSS) terminal inlets and piping in appropriate projects. The source for AGSS inlets shall connect to the medical vacuum system piping above the ceiling and downstream of the zone valve box serving the room.
9. Design flow rates at each terminal unit.
10. Calculate total flow for each medical gas system.
11. Ensure that all medical gases and vacuum systems are provided with both normal and emergency electrical power supply.
C. Design keys
1. Number of stations
The first step is to locate and count outlets/inlets, often called "stations" for each specific gas type. In fact, there is no code that mandates the exact number of stations in various areas of healthcare facilities. Therefore, this is usually done by the medical planner or the architect based on requirements of the facility.
2. Flow rates
Each station must provide a minimum flow rate to ensure proper functioning of connected equipment. The flow rates and diversity factors vary for individual stations depending on the total number of terminal units and the type of provided care. A diversity or simultaneous-use factor is used to allow for the fact that not all of the stations will be used at once. It is used to reduce the system flow rate in conjunction with the total connected load for sizing mains and branch piping to all parts of the distribution system. This factor varies for different areas of the facility. For example diversity factor for operating rooms and emergency rooms is 100 per cent, meanwhile for inpatient rooms is 10 per cent. In general, minimum flow rates can be estimated for any pipe section as: Oxygen- 200 L/min; Medical air- 200 L/min; Vacuum- 85 L/min; Nitrous oxide- 28 L/min; Carbon dioxide- 28 L/min; Nitrogen- 425 L/min.
3. Medical gases outlet/inlet terminals
Various types of medical gases outlet/inlet terminals are provided from different manufactures. The terminals are available in various gas sequence (e.g. O2, N2o, Air, etc.), center-line spacing, and concealed mounting. It is more practical to select terminals specifications to be complied with the adapters found on hospital's anesthesia machines, flow meters, vacuum regulators, etc.
References
1. K. G. Wentink, and R.D. Jackson ", Medial gas and vacuum systems," Plumbing Systems & Design, January/February 2006, pp: 44-53.
2. J. Dyro, "The clinical Engineering handbook", Elsevier press, NYK, 2004, pp: 537- 540.
3. "Medical vacuum and gas systems", The University of Texas, MD Anderson Cancer Center, 2010.
4. DH Estates and Facilities Directorate, "Health technical memorandum 02-01: Medical gas pipeline systems - part A design, installation, validation, and verification", May 2006.
5. DH Estates and Facilities Directorate, " Health technical memorandum 02-01: Medical gas pipeline systems - part B operational management", May 2006.
6. M. Abu Al-Ainin, " Medical gases pipeline systems MGPS", Nile University, Egypt, 2014.