
Obstructive sleep apnea syndrome is a common sleep disordered breathing which is caused by partial or complete upper airway collapse resulting in intermittent hypoxemia, sympathetic activation, and autonomic disturbances. OSAS leads to several cardiovascular complications like hypertension, myocardial infarction, arrhythmias, coronary artery diseases, pulmonary hypertension, and stroke. Early diagnosis in high-risk patients with polysomnography and treatment helps in decreasing morbidity and mortality associated with its complications.
Introduction
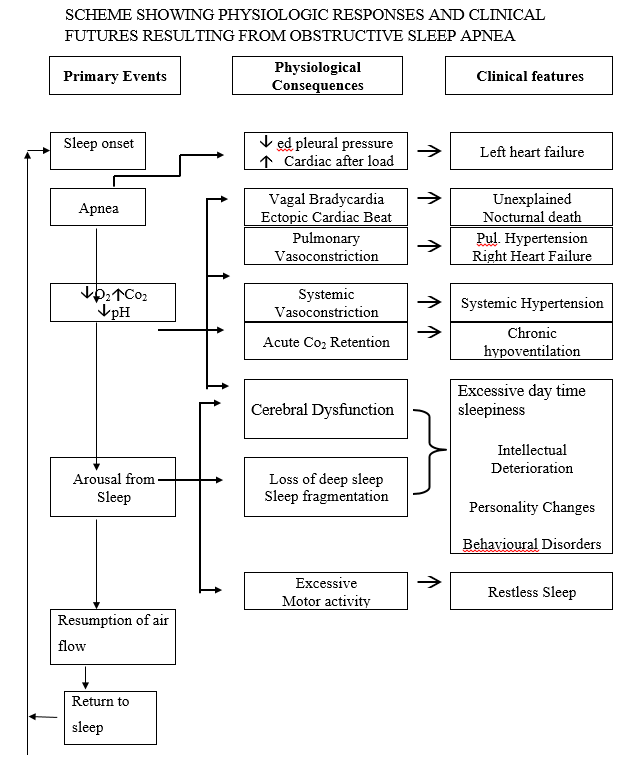
Obstructive sleep apnea syndrome (OSAS), also referred to as obstructive sleep apnea hypopnea syndrome (OSAHS) is a common sleep disorder that involves cessation or significant decrease in the airflow in the presence of breathing effort. Approximately 4 per cent men and 2 per cent women suffer from obstructive sleep apnea syndrome. It is a common sleep disordered breathing associated with upper airway collapse. Arousal from sleep is required to re-establish the airway patency. This distortion of sleep pattern and repetitive awakening contributes to excessive daytime sleepiness and other functional impairments like impaired cognition, memory and mood alterations. The nocturnal hypoxia may also lead to pulmonary and systemic hypertension as well as other cardiac and metabolic complications.
Cardiovascular complications are serious and common in OSAS as sympathetic drive is increased. These includes systemic hypertension, nocturnal arrhythmias, myocardial infarction, pulmonary hypertension, cor pulmonale and sudden nocturnal death.
BURDEN OF DISEASE (WORLDWIDE)
The prevalence of obstructive sleep apnea is approximately 4 per cent in men and 2 per cent in women.
BURDEN OF DISEASE (INDIA)
According to the Udwadia et al, a study done in Mumbai urban Indian male population, the estimated prevalence of SDB (AHI of 5 or more) was 19.5 per cent, and that of OSAHS (SDB with daytime hyper-somnolence) was 7.5 per cent. Sharma et al in a two-stage, cross-sectional, community-based prevalence study in a semi-urban community in Delhi showed prevalence rates of 13.74 per cent and 3.57 per cent, for OSA and OSAS, respectively.
Obstructive sleep apnea syndrome (OSAS): The obstructive sleep apnea syndrome (OSAS) is said to be present when the AHI is greater than 5 events per hour and the patient has symptoms of excessive daytime somnolence, unrefreshing sleep, or chronic fatigue OR when AHI is greater than 15 events per hour even in absence of symptoms.
Severity of OSAS:
Mild: AHI/RDI 5-15 events/hr
Moderate: AHI/RDI 15-30 events/hr
Severe: AHI/RDI more than 30 events/hr
Definition of terms related:
Apnea: Apnea is the cessation, or near cessation of airflow. It exists when airflow is less than 10 percent of pre-event baseline for at least 10 seconds in adults.
Hypopnea: Reduction of airflow to a degree that is insufficient to meet the criteria for an apnea. The most recent definition, recommends that hypopnea be scored when the following three criteria are met:
• Airflow decreases at least 30 percent from pre-event baseline
• The diminished airflow lasts for at least 10 seconds
• The decreased airflow is accompanied by at least 3 percent oxyhaemoglobin desaturation from pre-event baseline, or an arousal.
Respiratory event related arousal (RERA): A sequence of breaths that lasts at least 10 seconds, characterised by increasing respiratory effort or flattening of the nasal pressure waveform followed by an arousal from sleep, which does not meet the criteria for an apnea or hypopnea.
Apnea-hypopnea index (AHI): Number of apneas plus hypopneas per hour of sleep time.
Respiratory disturbance index (RDI): Number of apneas plus hypopneas plus RERAs per hour of sleep time.
Physiology:
Sleep is a period of bodily rest characterised by reduced awareness of the environment, a species-specific posture, and for most species, a particular sleep place. During each period of sleep, mammal’s cycle between two phases, non–rapid eye movement sleep (NREM) and rapid eye movement sleep (REM). NREM always precedes a bout of REM. In humans, the cycle length averages 90 min, although NREM and REM are not evenly distributed through the night. Cycle length varies directly with brain weight; hence, the family dog or cat cycles between NREM and REM more frequently, about every 25 minutes, as well as having multiple sleep periods.
Obesity is the primary risk factor for the development of Obstructive Sleep Apnea Syndrome (OSAS) and contributes to cardiovascular and metabolic abnormalities in subset of population. Periodic apneas and hypopneas during sleep result in intermittent hypoxemia, arousals, and sleep disturbances. These pathophysiological characteristics of Obstructive sleep apnea (OSA) are likely mechanisms underlying cardiovascular and metabolic abnormalities including hypertension and other cardiovascular diseases, altered adipokines, inflammatory cytokines, insulin resistance and glucose intolerance.
PATHOPHYSIOLOGY OF OSAS
Conceptually, the upper airway (UA) is a compliant tube and, therefore, is subject to collapse. OSA is caused by soft tissue collapse in the pharynx.
Trans-mural pressure is the difference between intraluminal pressure and the surrounding tissue pressure. If trans-mural pressure decreases, the cross-sectional area of the pharynx decreases.
Anatomic factors (e.g., enlarged tonsils, volume of the tongue, soft tissue, or lateral pharyngeal walls); length of the soft palate; abnormal positioning of the maxilla and mandible) may each contribute to a decrease in the cross-sectional area of the upper airway and/or increase the pressure surrounding the airway, both of which predispose the airway to collapse.
Neuromuscular activity along with reflex activity decreases during sleep. It is more pronounced in OSA. This leads to decrease motor output to upper airway muscles leading to partial or complete collapse of upper airways.
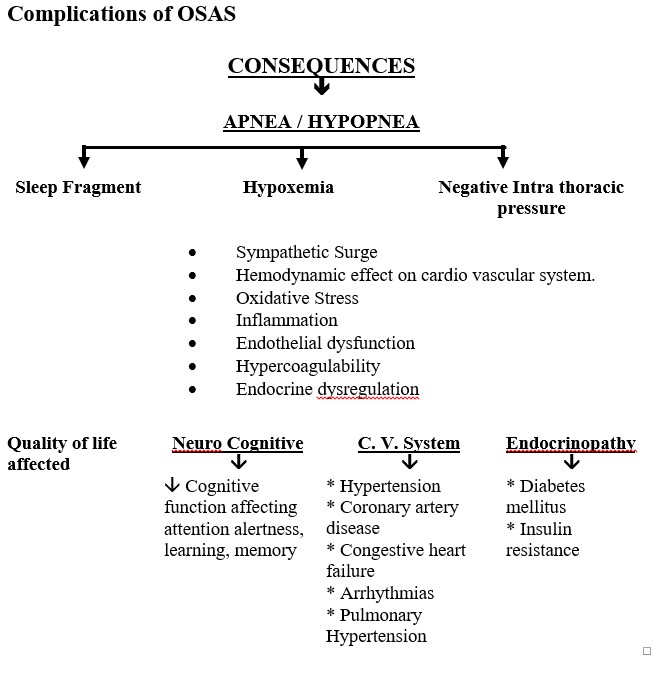
Pathophysiological mechanisms leading to cardiovascular diseases
OSA patients have intermittent hypoxemia and carbon dioxide retention that alters the autonomic and haemodynamic responses to sleep. The frequent cardiovascular stressors during apnoea and hypopnoea over the years contribute to the development of chronic cardiovascular diseases. Pathophysiological mechanisms involved are sympathetic activation, cardiovascular variability, activation of systematic inflammatory pathways, oxidative stress, endothelial dysfunction, intrathoracic pressure changes and hemodynamic instability.
SYMPTOMS OF OSA
• Loud, habitual snoring
• Witnessed apneas
• Nocturnal awakening
• Gasping or choking episodes during sleep
• Nocturia
• Unrefreshing sleep, morning headaches
• Excessive daytime sleepiness
• Automobile or work-related accidents
• Irritability, memory loss, personality change
• Decreased libido
• Impotence
DIAGNOSIS OF OSA
The most common among the SBD is OSA. Diagnostic criteria for OSA are based on clinical signs and symptoms determined during a comprehensive sleep evaluation, which includes a sleep history and patients’ physical examination.
History and clinical examination should be in three settings. First as part is the routine health maintenance evaluation, second as part is symptomatic evaluation for OSA and third part is comprehensive evaluation of patients with high risk for OSA (obesity, hypertension, diabetes mellitus, atrial fibrillation etc.).
The risk factors for OSAS are:
o Gender (male/female 2:1)
o Obesity (>120 per cent ideal body weight)
o Neck size (collar size >17 inches in males, >15 inches in females)
o Upper airway anatomy
o Specific genetic diseases, e.g., Treacher Collins, Down syndrome, Apert’s syndrome, Achrodorophsia, etc.
o Genetic factors
o Endocrine disorders—hypothyroidism, acromegaly
o Alcohol, sedative or hypnotic use
In the physical examination of patient, attention should be paid to the presence of obesity, body mass index, neck circumference, signs of upper airway narrowing, Modified Mallampati score, retrognathia/micrognathia, lateral peritonsillar narrowing, macroglossia, tonsillar hypertrophy, elongated/enlarged uvula, high arched/narrow hard plate, nasal abnormalities (deviated nasal septum, polyps, turbinate hypertrophy).
The next step to reach the diagnosis after history and physical examination is the Polysomnography (sleep study).
POLYSOMNOGRAPHY (SLEEP STUDY)
It is a diagnostic test for sleep disordered breathing. The level of sleep study is decided by the number of parameters recorded with the help of channels of electrodes applied to the patient for study.
Types of sleep study:
Level 1: In hospital or sleep laboratory, fully attended by sleep technician with more than 7 channels.
Level 2: In hospital or sleep laboratory, unattended with more than 7 channels.
Level 3: Home sleep study with 4-7 channels.
Level 4: Only few parameters are studied with oximetry as one parameter
Level 1 overnight polysomnography (PSG) which is done in hospital or in sleep laboratory, attended by trained technician is the “Gold standard” for evaluation of sleep-disorders
Treatment of OSAS:
Medical management
1. Weight reduction- reduction in 10 per cent of body weight decrease AHI by 20 per cent. Weight reduction also helps in decreasing the CPAP pressures.
2. Avoidance of alcohol, sedatives and nicotine
3. Sleeping in lateral position decreases the AHI as most of apneas and hypopneas are in supine position
4. Treatment of nasal obstruction
5. Sleep hygiene-
• Go to bed at the same time each night and get up at the same time each morning, including on the weekends
• Make sure your bedroom is quiet, dark, relaxing, and at a comfortable temperature
• Remove electronic devices, such as TVs, computers, and smart phones, from the bedroom
• Avoid large meals, caffeine, and alcohol before bedtime
• Get some exercise. Being physically active during the day can help you fall asleep more easily at night.
Pharmacotherapy: none of the drugs are approved for treatment of OSA
Positive Airway Pressure therapy: It is the mainstay for treatment of OSA. Positive airway pressure acts as a stent and prevent collapse of upper airways. Compliance is the major issue. It improves the quality of life and decreases complications and mortality. CPAP mode is usually advised, but Bi level PAP or Auto PAP can be given. Bilevel PAP is considered better in obesity hypoventilation syndrome or overlap syndrome
Oral appliances: They are indicated for patients with mild to moderate OSA. Patients who do not prefer CPAP, or who do not respond to CPAP/BiPAP treatment. Mandibular repositioning/advancing appliance (MRA) and tongue retaining appliances (TRA). Both these appliances help increasing upper airway space thus preventing collapse during sleep.
Surgical management: Surgical management is indicated only if upper airway obstruction is present of BMI is very high. Nasal surgery (correction of anatomical defects), Maxillo-mandibular surgeries which include maxillo-mandibular advancement, genioglossus advancement, distraction osteogenesis and uvulopalatopharyngoplasty (UPPP) for retropalatal obstruction. Bariatric surgery is indicated in patients with BMI ≥ 35kg/m. Gastric bypass is the most successful procedure and gastric banding is the least effective procedure for treating OSA.
References: