The Covid pandemic has on one hand, increased patient hesitancy towards physically visiting a health care facility, and on the other increased the need for healthcare support. The field of telemedicine, in which clinicians use remote evaluation and monitoring to diagnose and treat patients, has leapfrogged in the last two years. The World Health Organization (WHO) defines Telemedicine as, “The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.” The role of telemedicine in disaster management and pandemic control was understood by the health care systems and anticipating the increased need of telemedicine by health-care providers, the Medical Council of India released practice guidelines in March 2020.These guidelines changed the face of Indian health care and the pandemic handling. They defined the diverse roles of telemedicine in acute care medicine settings, including virtual intensive care unit (ICU) care, after-¬hours medical admissions, and, most aptly, disaster management.

At Medanta hospitals, enabling delivery of remote, safe healthcare, the use of telemedicine rapidly scaled up during COVID. Telemedicine made quality healthcare more accessible and transparent, and ensured inclusivity and equality of access. Increased use of electronic diagnostic devices like electronic stethoscope, BP, and SPO2 monitors enabled doctors to engage in virtual consultation and remote monitoring of patient health. Telemedicine facilitated staffing of facilities that found themselves overwhelmed with pandemic-related patient overload. This helped in easing the pressure the increased covid admissions put on an already stretched healthcare system.
Telemedicine changed the way chronic care is delivered at a time when people are hesitant of stepping out of their homes to seek medical care. Telemedicine can be used for ongoing management of chronic diseases such as bronchial asthma, hypertension, and diabetes mellitus, patients who need regular dose adjustments, no more need to travel to the hospital physically to consult their doctor. They can easily do so from the safe confines of their home through a simple mobile device. This has helped maintain the continuity of care amidst the pandemic. As patients and doctors get increasingly comfortable with virtual consultations, this may well become a norm in the near future.

In addition, healthcare systems leveraging telemedicine for patient care will gain several advantages, including workforce sustainability, reduction of provider burnout, limitation of provider exposure, and reduction of personal protective equipment (PPE) waste. We utilised commercial telemedicine carts on-site at hospitals and laptops at home. Doctor workstations were enabled by adding web cameras to the existing workstations and purchasing additional laptops for new telemedicine providers. This made telemedicine a comfortable choice for both the user and the provider.
A feedback survey regarding the use of teleconsultations at Medanta revealed that both doctors and patients were satisfied with the experience. The Information Technology team was able to ensure ease of appointments and good quality of audio and visual support. Patients were comfortable with the punctuality of doctors and the time spent in the consult along with the explanation of treatment process. The comfort and privacy of this consultation was most appreciated by the patients. The initial experience of doctors included some concerns around inappropriate dressing by patients and attendants but his
changed over time, when instructions were shared with patients. The overall patient rapport and communication was appreciated by the doctors.

It was interesting to note that the gender and age distribution was well represented, this surely emphasizes the fact that it was easy to use and therefore the acceptance of this technology was high in the population independent of age or gender. The use of the technologies did not vary over tier 1, 2 or 3 cities, with access of the internet reaching the hinterland, patients all over the country were comfortable using telehealth technologies.

Diagnosis and treatment: Telemedicine increases efficiency and the quality of care, reduces unnecessary patient transport, decreases exposure in the time of the pandemic and increases physicians’ and patients’ satisfaction
Monitoring: Telemedicine can be used for ongoing management of chronic diseases such as respiratory, cardiac, liver and kidney diseases; particularly during a time when social distancing is encouraged. It can play an important role in also providing psychological support to patients and their family members without getting exposed to the infection. Telemedicine also expanded support by helping train care providers of the elderly, young children and other dependents
Community paramedicine: Community paramedicine is a new and evolving healthcare model. It allows paramedics and emergency medical technicians (EMTs) to operate in expanded roles by assisting with public health and primary healthcare and preventive services to underserved populations in the community. This is being tested along with telemedicine models in providing remote vaccination, and continued care for Tuberculosis and other chronic diseases in the remote community. Telemedicine has also helped in shouldering the challenge of health care during massive public gatherings, for example during Maha Kumbhamelas through Mobile Telemedicine system vans equipped with videoconferencing systems for visual communication enabling doctors in remote places connect to any of the telemedicine-enabled medical hospital and super speciality hospital for expert opinions.
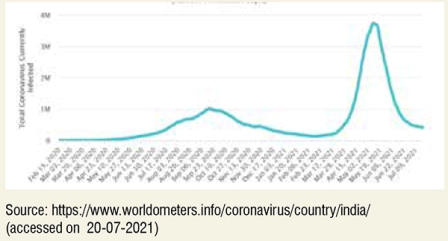
Trends of increased teleconsultation use overlapped with the covid wave patterns over the two major waves seen in India. This brings to focus that despite comfort with telemedicine, patients may revert to in-person visits when the pandemic subsides. A change in practice towards use of telemedicine even during a nonpandemic condition will need Information-Education – Communication (IEC) modules that will help hospitals in connecting with new patients and providing continued care to the old one.
Although telemedicine holds promise for pandemic response, this technology has limitations. It requires robust IT infrastructure, training of both nurses and physicians, and modifications to integrate within hospital workflows. Major barriers encountered included cost, and equipment functionality. However, close coordination with executive leadership, and robust IT support, we were able to move past these obstacles in expanding our telemedicine infrastructure for support during this crucial time.

The institutional best practices of Indian hospitals must be shared and policy-makers must take advantage of the telemedicine experiences reported during this outbreak to further define the practices of e-healthcare under laws of privacy and data protection.
The greatest hope for use of telemedicine technology is that it can bring the expertise to remote medical practice and provide an opportunity for standardisation and equity in provision of healthcare, both within individual countries and across regions and continents. Combined with geotracking it can play a pivotal role in anticipating epidemics and real-time monitoring of diseases. With preventive and promotive health becoming even more critical in these times telemedicine can be an important tool for health communication and disease prevention, relaying relevant information, enabling informed decision-making, improving health care communication process, create support systems and promote self-care and domiciliary care practices.