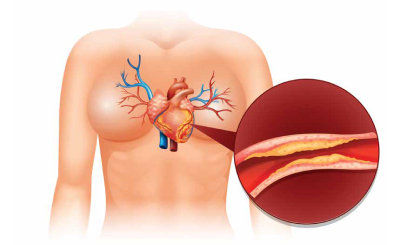
Aortic stenosis (AS) is a prevalent cardiac valve pathology, particularly in the elderly population, and is associated with increased morbidity and mortality. Common risk factors for AS include ageing, smoking, hypertension, and hyperlipidemia. AS is characterised by progressive valvular leaflet calcification, inflammation and lipid accumulation, resulting in rigidity, immobility and reduced leaflet opening. Additionally, left ventricular hypertrophy is frequently observed in patients with AS. Even in asymptomatic severe patients, the likelihood of cardiac mortality and need for surgical aortic valve replacement increases over time. Patients with severe AS face an elevated risk of developing major adverse cardiovascular events (MACE) after major non-cardiac surgery (NCS). While AS has been associated with high perioperative mortality, recent studies indicate a potential decrease in mortality rates.
Accurate preoperative assessment plays a crucial role in identifying high-risk patients and implementing appropriate management strategies. Preoperative assessment of AS involves evaluating the severity of AS and considering concurrent conditions, particularly coronary artery disease (CAD) and chronic kidney disease (CKD).
Transthoracic echocardiography (TTE) is a valuable non-invasive tool for assessing AS severity, left ventricular systolic and diastolic function, left ventricular hypertrophy, and other valvular diseases. Current guidelines recommend perioperative TTE for patients with known AS to determine appropriate perioperative management, if echocardiography has not been performed within the past 12 months or if there have been significant changes in clinical status or physical examination since the prior evaluation. Progression of AS leads to an average annual increase in the transaortic pressure gradient of approximately 3mmHg per year and decrease in the aortic valve area by 0.3 cm2. It is recommended that the transaortic gradient be measured when the patient is normotensive, as systemic hypertension can augment valve obstruction and reduce forward flow, potentially leading to an underestimation of the severity of valvular disease.
Concomitant diseases, such as coronary artery disease (CAD) and chronic kidney disease (CKD), should also be evaluated. CAD frequently coexists in patients with AS. CKD has a higher prevalence in patients with AS and is correlated with increased mortality. Baseline renal function should be assessed, as it is an important factor in determining the risk of acute kidney injury (AKI) after aortic valve replacement (AVR).
Patients with severe AS patients are at an increased risk of major adverse cardiovascular events (MACE), primarily due to hypotension and tachycardia induced by anaesthesia and surgical stress. Unforeseen surgical site bleeding can further worsen hemodynamics. A meta-analysis including just under 30,000 patients demonstrated that both symptomatic and asymptomatic AS patients were associated with an increased risk of myocardial infarction and MACE, without increased mortality. In a study, comparing severe AS patients who had and had not undergone AVR prior to non-emergent/non-urgent major non-cardiac surgery, higher rates of blood transfusions, hemodynamic monitoring, and catecholamine use were seen in those patients who did not undergo antecedent AVR. Increased MACE, driven primarily by a higher incidence of heart failure, was seen amongst severe AS patients undergoing major NCS without antecedent AVR. However, there was no increase in the incidence of myocardial infarction or 30-day mortality regardless of whether or not AVR was performed prior to NCS. Limited evidence suggests that major NCS may accelerate the progression of AS, but further studies are needed.
The estimation of cardiovascular morbidity and mortality in patients requires consideration of both individual comorbidities and the type of procedure or surgery. Surgical-related risks are determined by the nature and duration of the operation, and surgical risk assessment tools may be utilised to evaluate 30-day risk of cardiovascular mortality, myocardial infarction, and stroke. Tashiro et al identified need for emergency surgery, atrial fibrillation and kidney disease (serum creatinine>2mg/dL) as predictors of worse outcomes in patients with severe AS undergoing NCS. Similarly, Agarwal et al. also identified high-risk NCS, symptoms related to severe AS, coexistent moderate or severe mitral regurgitation, and known CAD as predictors of MACE at 30-days in AS patients undergoing major NCS.
The 2020 ACC/AHA guidelines for management of patients with valvular heart disease provide numerous recommendations for aortic valve intervention in patients with severe AS, including Class I recommendations for intervention in symptomatic patients and those with reduced left ventricular systolic function (defined as LVEF <50 per cent). Severe AS patients meeting guideline indications for intervention should consider proceeding with aortic valve intervention prior to NCS, due to longer term prognostic implications related to their aortic valve disease and independent of their need for NCS. Asymptomatic patients with severe AS who do not have left ventricular dysfunction may consider elective NCS without prior aortic valve intervention, although close hemodynamic monitoring is recommended. Delaying NCS may be inappropriate in certain scenarios, such as aggressive malignancies, and proceeding with NCS may be reasonable in understanding the elevated risk of postoperative heart failure, albeit without a significant increase in periprocedural cardiac mortality.
Where aortic valve replacement is pursued prior to NCS, the choice between surgical and transcatheter aortic valve replacement depends on a variety of factors including patient characteristics, age, comorbidities, and vascular access. Post-aortic valve recovery time prior to NCS may be an important consideration, and transcatheter AVR may allow a shorter convalescence prior to proceeding with NCS. Aortic balloon valvuloplasty may be considered for short-term relief of AS prior to NCS in patients who are poor surgical or procedural candidates for aortic valve intervention.
The perioperative management of patients with AS undergoing NCS requires careful assessment, risk stratification and consideration of aortic valve intervention strategies. Routine preoperative assessment should include transthoracic echocardiography, as well as evaluation for CAD and CKD. While NCS may be performed safely with close hemodynamic monitoring in asymptomatic patients with preserved left ventricular systolic function without preceding aortic valve replacement: patients with indications for aortic valve intervention based on current valvular heart disease guidelines should be considered prior to NCS.