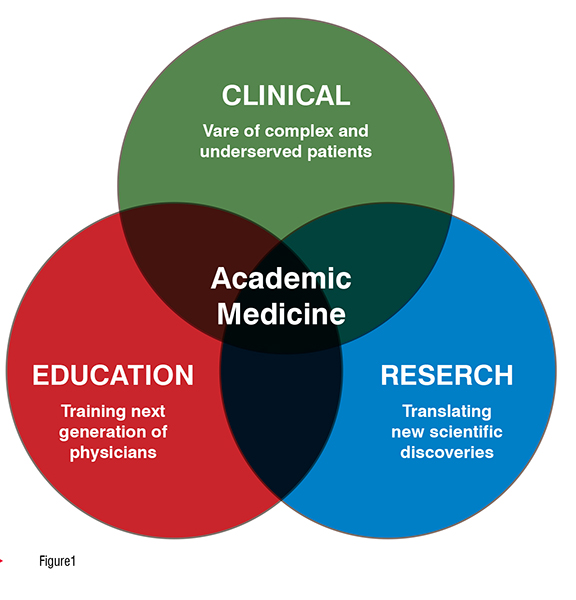
Academic medicine is founded on the tripartite principles of clinical care, education, and research. Radiology—the study of medical images—exemplifies the “bench-to-bedside” translation crucial for advancement in the field. In this article, we summarise foundational concepts, drivers, and implications for the future of health care.
Academic health centres follow the tripartite mission of advancing clinical care, education, and research. Academic physicians have the opportunity to pursue focused excellence in clinical and translational research, medical education, safety and quality, global health, health care informatics, and public advocacy. (Figure 1)
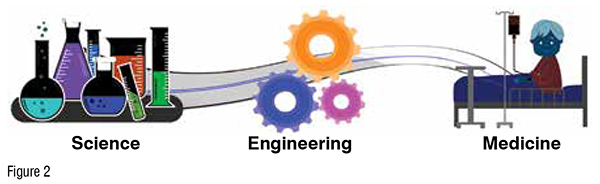
A key step in information flow involves the conduction of research ideas into practice, moving scientific concepts from “bench-to-bedside.” Using the RDI (research-developmentinnovation) model, fundamental knowledge discovery is utilised to improve processes and advance patient care. This process requires continual communication and feedback among basic scientists, engineers, and physicians. (Figure 2)
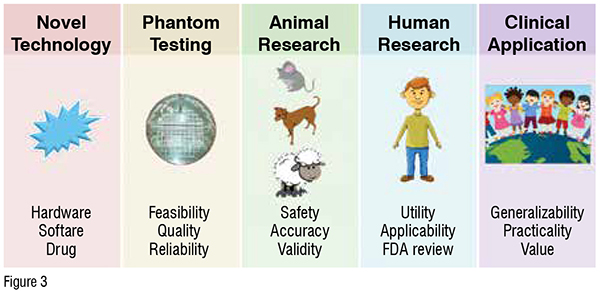
In radiology, stepwise development and implementation of novel technologies is an important aspect of evidence-based care. Continual innovation pressures and the advent of disruptive technologies such as automation, cloud computing, and blockchain are transforming the modern marketplace. Ongoing advances in radiology include innovations in hardware (scanner platforms), software (acquisition techniques and post-processing), and pharmaceuticals (contrast agents and radiotracers). Most imaging technologies are initially tested on phantoms and animal models, then move to human subjects pilot evaluation for FDA review. Ultimately, product practicality, generalisability, and added value are key determinants of whether the product will be effectively integrated into clinical practice. (Figure 3)
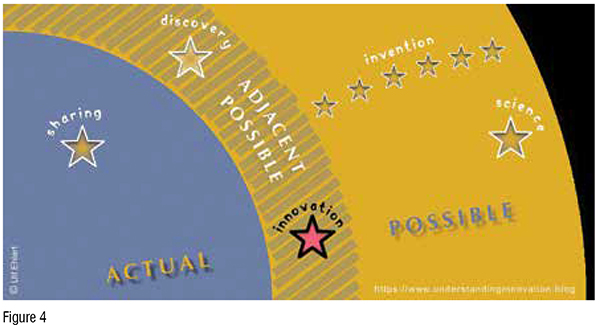
The notion of the “adjacent possible” represents society’s next great discovery, arising from the confluence of current knowledge and state-of-theart advances. (Figure 4)
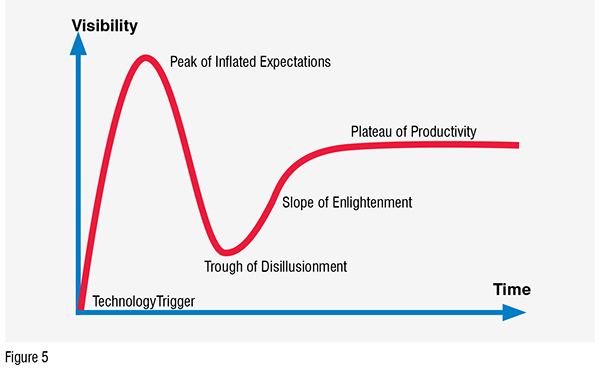
However, public sentiment for new technologies varies over time, following the Gartner hype cycle: initial peak of inflated expectations, subsequent trough of disillusionment, gradual slope of enlightenment, and eventual plateau of productivity. In order to facilitate steady progress and forward thinking in medicine, physicians need to actively “challenge the dogma” by building multidisciplinary networks to promote collision science. (Figure 5)
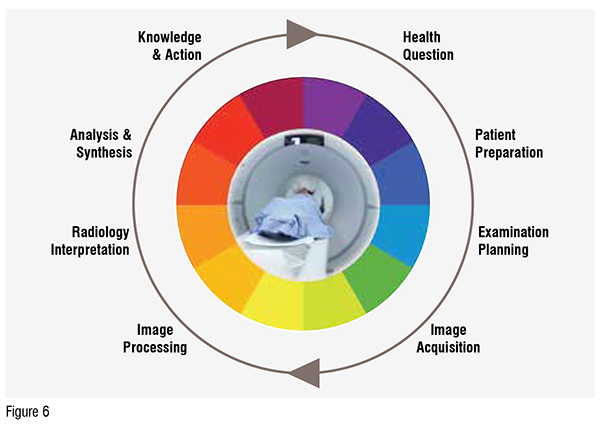
In radiology, process improvement strategies follow the imaging care cycle. Patients are referred to radiology for a specific health question, prompting a specific imaging examination and protocol. Using a “lean” approach, departments can continuously optimise and streamline each stage of the imaging life cycle. (Figure 6)
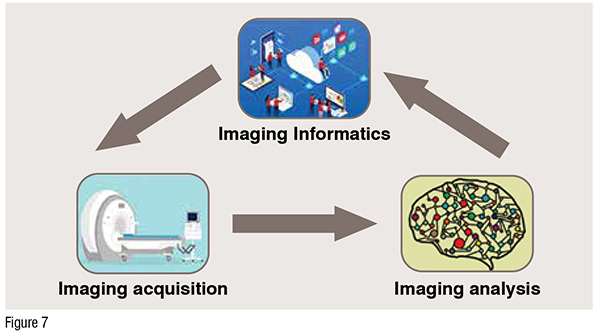
The translational imaging (I3) model helps to conceptualize data flow through the radiology department via three core pillars of imaging acquisition, imaging analysis, and imaging informatics. (Figure 7)
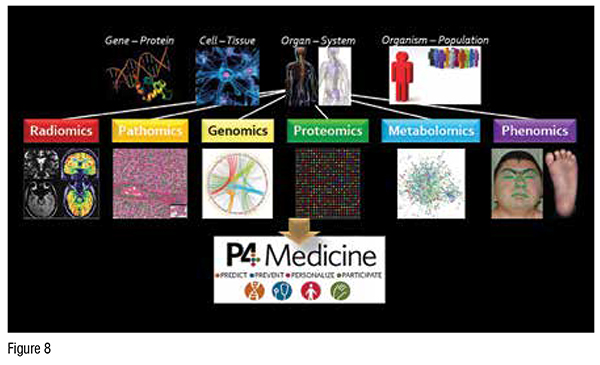
The grand vision of precision (P4) health integrates multiscale biological information extracted from various disciplines of medicine, including radiology, pathology, genomics, clinical examination, and laboratory values. The ultimate goal of P4 health is to achieve better risk screening and disease prevention, earlier and more accurate patient diagnosis, personalised care and treatment regimens, and fully participatory decision making among patients and clinicians. (Figure 8)
Being a highly data and technologydriven specialty, radiology is a major driver of health care. A radiologist serves as the “doctor’s doctor,” providing important advice and insights to referring clinicians to guide patient diagnosis and management. However, radiologists are not directly patientfacing; as consultants to multiple stakeholders, their contributions can be overlooked by patients and the public. Opportunities for radiologists to engage with referring clinical teams include multidisciplinary care conferences, integrated clinics, inpatient radiology rounds, and consult services. Major pillars of excellence at leading hospitals centre on oncology, neuroscience, cardiovascular, immunity, women’s and children’s care—all areas in which imaging plays a critical role. (Figure 9)
During the COVID-19 pandemic, agile management and disaster response have inspired transformational changes in health care operations and delivery, particularly in the arena of digital health. Developing reliable systems infrastructure is particularly important in ensuring sustainable growth and development. Academic medical centers can continue fostering innovation through interdisciplinary programs with other hospital and university departments, as well as strategic publicprivate partnerships. Entrepreneurial incubators and accelerators can help provide startup funding and commercial sponsorship for new companies.
Radiology is poised to lead the field of telemedicine, having already developed international DICOM standards (Digital Imaging and Communications in Medicine) and interoperable PACS (picture archiving and communication system) for medical image display, interpretation, storage, and transmission. Much like the Six Million Dollar Man, medical imaging technology continues to become “better, faster, and stronger.” Magnetic resonance imaging (MRI), the crown jewel of diagnostic imaging, is undergoing a paradigm shift from the conventional (1.5 Tesla) and highfield (3 Tesla) platforms seen in most hospitals. Ultrahigh-field (7 Tesla) MRI is now Food and Drug Administration (FDA)-approved for all major MRI vendors. Ultrahigh-field imaging enables interrogation of microscopic and mesoscopic biological processes, extending our understanding beyond traditional macroscopic anatomy. (Figure 10)
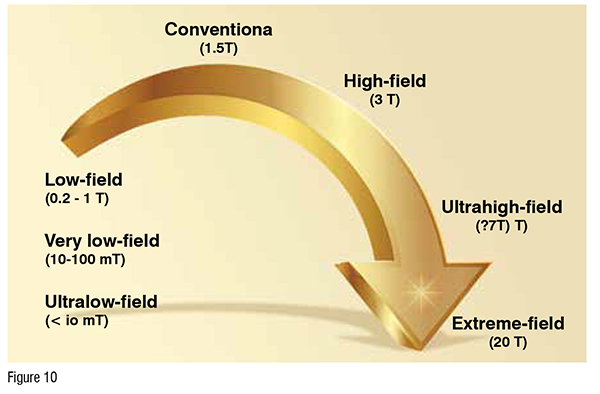
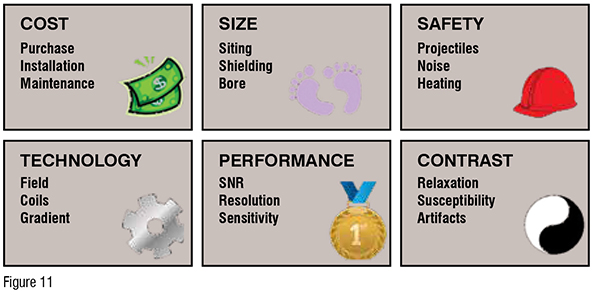
Meanwhile, low-field MRI units are leveraging lower cost and smaller footprints to enable broader accessibility to rural areas and underserved populations. (Figure 11)
Finally, software advances including artificial intelligence (AI) are enabling radiologists to “do more with less” by optimising workflow processes; minimising imaging time, patient radiation, and contrast doses; and extracting high-quality, reliable, and accurate diagnostic information. 3D visualisation (virtual, augmented, and mixed reality) facilitate patient counselling, medical education, surgical planning and guidance.
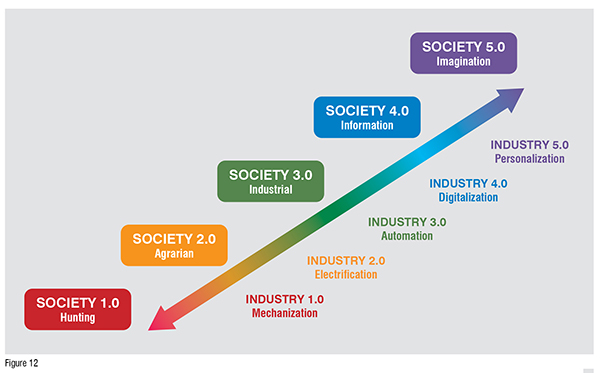
The nature of work has changed over time, as humans evolved from a huntergatherer society and underwent the 1st through 4th industrial revolutions of mechanisation, electrification, automation, and digitalisation. The ongoing COVID-19 pandemic has accelerated global development of big data and the internet of things, with machines replacing much of traditional human work. We are rapidly entering the 5th industrial revolution, with personalised human-machine collaborations that maximise creativity and collective intelligence. (Figure 12)
Modern health care parallels society’s increasing focus on technology and big data, accelerated by the global pandemic. As data and technology stewards, radiologists have an incredible opportunity to influence the future of medicine. Artificial intelligence is empowering faster, better, and safer imaging with end-to-end workflow optimisation and performance augmentation, freeing up radiologists’ time to maximise cognitive potential and serve as valuable consultants on difficult cases. Important future AI tools will include study triage, error minimisation, clinical decision support, structured reporting and communication, and business analytics. Big data informatics is guiding precision education with standardised and tailored curricula that address the shifting global workforce. International 5G connectivity is enabling democratisation of care with multicentre expert consultations, remote-control imaging, and robotic surgeries. Smart devices and wearable sensors are realising the potential of preventive care with real-time monitoring, point-of-care-diagnostics, biofeedback, and telemedicine consults.
As we move toward precision theranostics (therapeutics + diagnostics), integrated patient datasets will guide the selection of targeted therapies to achieve best outcomes. In this exciting future, radiologists will serve as central consultants for enterprise imaging and continued drivers of technology and innovation. Together, we can build the ultimate “imagination” society and realise humanity’s greatest potential.