This article explores the pivotal role of nuclear imaging systems in precision medicine, discussing their applications in cancer diagnosis, cardiovascular assessment, neurological disorders, therapeutic monitoring, and molecular imaging. It highlights technological advancements, challenges such as cost and radiation exposure, and the promising future of nuclear imaging in improving patient outcomes.
Introduction:
Precision medicine represents a transformative approach in healthcare, tailoring treatments and interventions to individual patients based on their unique genetic makeup, lifestyle, and environmental factors. At the heart of this revolution are advanced technologies like nuclear imaging systems, which play a pivotal role in diagnosing, monitoring, and treating various medical conditions. This article delves into the intricacies of nuclear imaging systems, their applications in precision medicine, technological advancements, challenges, and future prospects.
A. Understanding Nuclear Imaging Systems
Nuclear imaging encompasses a range of techniques that utilize radioactive tracers to visualize and assess the function of organs, tissues, and physiological processes within the body. These techniques include positron emission tomography (PET), single-photon emission computed tomography (SPECT), and hybrid imaging modalities like PET-CT and SPECT-CT. The principle behind nuclear imaging involves administering radiopharmaceuticals, which emit gamma rays or positrons that are detected by specialized cameras to create detailed images.
B. Applications in Precision Medicine
a. Cancer Diagnosis and Staging: Nuclear imaging plays a critical role in oncology by accurately detecting tumors, evaluating their metabolic activity, and determining the extent of metastasis. PET scans with radiotracers like fluorodeoxyglucose (FDG) are widely used to diagnose and stage various cancers, aiding clinicians in designing personalized treatment plans.
b. Cardiovascular Assessment: Nuclear imaging techniques are invaluable in assessing cardiac function, blood flow, and myocardial viability. SPECT imaging with radiotracers such as technetium-99m (Tc-99m) allows for non-invasive evaluation of coronary artery disease, myocardial perfusion defects, and post-infarction myocardial viability, guiding interventions and optimizing patient outcomes.
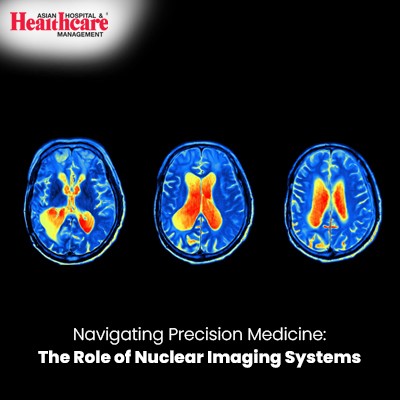
c. Neurological Disorders: PET imaging, particularly with tracers like fludeoxyglucose (FDG) and amyloid imaging agents, contributes significantly to the diagnosis and management of neurodegenerative diseases such as Alzheimer's and Parkinson's. These scans provide insights into brain metabolism, amyloid plaque deposition, and neuronal function, aiding in early detection and disease monitoring.
d. Therapeutic Monitoring: Nuclear imaging is instrumental in monitoring response to therapy, especially in cancer patients undergoing chemotherapy or radiation therapy. PET scans can assess treatment efficacy by measuring changes in tumor metabolic activity, guiding treatment modifications and improving patient care.
e. Molecular Imaging: Advances in molecular imaging techniques, including targeted radiopharmaceuticals and theranostics, enable precise characterization of biomarkers, receptor expression, and molecular pathways involved in disease pathogenesis. This molecular-level information is vital for personalized treatment strategies and therapeutic decision-making.
C. Technological Advancements
Recent years have witnessed significant technological advancements in nuclear imaging systems, enhancing their capabilities and clinical utility in precision medicine:
a. Improved Image Resolution: High-definition PET and SPECT scanners with enhanced spatial resolution provide sharper images, improving diagnostic accuracy and anatomical localization.
b. Multimodal Imaging Integration: Hybrid imaging platforms such as PET-CT and PET-MRI combine functional and anatomical information, offering comprehensive assessments and precise localization of abnormalities.
c. Quantitative Analysis Tools: Software algorithms for quantitative analysis of nuclear imaging data enable precise measurement of physiological parameters, metabolic rates, and biomarker expression, facilitating objective disease characterization and treatment response assessment.
d. Radiotracer Development: Ongoing research in radiopharmaceutical development has led to the creation of novel tracers targeting specific molecular pathways, allowing for personalized imaging and targeted therapy delivery.
e. Artificial Intelligence (AI) Integration: AI-driven image reconstruction, analysis, and interpretation algorithms enhance diagnostic accuracy, streamline workflow, and support data-driven clinical decision-making in nuclear medicine.
D. Challenges and Future Directions
Despite the remarkable advancements, nuclear imaging faces several challenges in its integration into routine clinical practice:
a. Cost and Accessibility: The initial investment and operational costs associated with nuclear imaging systems can be prohibitive, limiting access in resource-constrained settings and underserved regions.
b. Radiation Exposure: Concerns regarding radiation exposure, particularly in pediatric and young adult populations, necessitate dose optimization strategies and adherence to stringent safety protocols.
c. Data Integration and Interoperability: Seamless integration of nuclear imaging data with electronic health records (EHRs) and other clinical information systems is essential for comprehensive patient management and data-driven decision support.
d. Regulatory and Reimbursement Landscape: Evolving regulatory frameworks and reimbursement policies pose challenges in adopting novel imaging technologies and ensuring sustainable financing models for nuclear medicine services.
e. Research and Collaboration: Continued research collaboration among academia, industry, and healthcare providers is crucial for advancing nuclear imaging technologies, validating clinical applications, and translating research findings into clinical practice.
Looking ahead, the future of nuclear imaging in precision medicine is promising, driven by innovations in radiotracer development, AI integration, and personalized therapeutic approaches. Collaborative efforts among stakeholders, along with ongoing investments in infrastructure and education, will pave the way for harnessing the full potential of nuclear imaging in improving patient outcomes and advancing precision healthcare.
Conclusion:
Nuclear imaging systems are at the forefront of precision medicine, offering insights into molecular processes, disease pathways, and individualized patient responses to therapy. From oncology to cardiology, neurology, and beyond, these advanced imaging techniques play a pivotal role in diagnosis, treatment planning, therapeutic monitoring, and research endeavors. As technology continues to evolve and interdisciplinary collaborations flourish, nuclear imaging holds immense promise in shaping the future of healthcare, driving personalized interventions, and improving patient outcomes in an era of precision medicine.