Medical imaging devices play a significant role in disease diagnosis. However, due to theories of operation, this class of devices pose high risk for patients, users, and environment. In this article, the basics of radiological safety and risk management are provided. In application, three modalities of medical imaging devices are presented.
Risk management is an organised process to identify and manage probable risks[1]. This definition implies four steps for risk management, namely:identification, assessment, control, and monitoring[1,2]. In fact, this strategy encompasses numerous procedures to mitigate or eliminate the possible risks. In healthcare facilities, risk management recently has become a mandatory requirement based on ISO/IEC 60601 standard[1]. Indeed, many entities in the hospital environment such as infrastructure, entire environment, and medical technology pose risk, which in turn must be managed properly[3]. Several studies have been conducted in these perspectives. According to the aim of this article, risk management for medical technologies, particularly, medical imaging devices is highlighted.
Medical imaging is a non-invasive procedure able to diagnosis human diseases. From this point, many imaging devices or modalities are utilised to identify and facilitate patient treatment protocol. Moreover, picture guided interventional methods are also used to guide specialists in some surgical procedures. There are common forms (modalities) of diagnostic imaging devices that employ various technologies to generate images for specific purposes. These modalities of radiology include conventional radiology (X-ray), fluoroscopy, angiography, mammography, Computed Tomography (CT), ultrasound/doppler, Magnetic Resonance Imaging (MRI), and nuclear medicine[4 in abs.]. Although medical imaging devices are the front line of the basic diagnosis in healthcare services, they are considered a source of high risk in terms of technology and application. In this context, radiation safety, electrical hazards, and overdose control are commonly conducted in the literature[5].
1. Classification of Radiation
Radiation is classified as ionising and non-ionising depending on its ability to ionise matter. In definition, non-ionising radiation cannot ionise matter, whereas ionising radiation can ionise matter either directly or indirectly. Typically, the minimum energy required to ionise an atom, i.e. to remove an electron is known as the ionisation potential[6]. Examples of non-ionising radiation are microwave, radio, and ultraviolet, meanwhile x-ray, beta, andgamma radiations are for ionising radiation. Figure 1 shows frequency spectrum of the electromagnetic waves. Forms of ionising radiation are categorized into
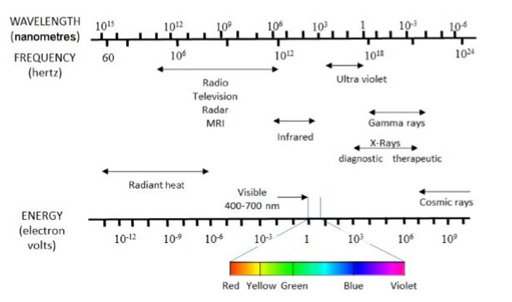
Fig.1 The electromagnetic spectrum [6]
2. Hazards of Radiation
Obviously, radiation is a significant health hazard in all hospitals.When radiation is present, high energy particles pass through human body. This effect can kill cells or even damage the DNA within cells which may lead to uncontrolled cell division. Indeed, type of hazard depends on type of radiation. In normal circumstances, 80 per cent of our exposure to non-ionising radiation is due to natural sources (radon gas), while 20 per cent comes from man-made sources (X-rays)[7]. Therefore, in case of non-ionising radiation, associated risk can be reduced by limiting exposure to radiation based on source of the radiation such as wearing eye google in laser applications. Also, microwave-based applications should be periodically monitored using appropriate measurement equipment. Biological hazards take place when exposure to radiation exceeds 0.5Gy over a period of time. Hazards of ionising radiation can be categorised into acute effects and latent effects. Symptoms of acute effects are nausea, vomiting, hair loss, and reddening of skin, whereas for latent effects are cataracts, genetic effects, and cancer[8].
3. Engineering factors for reducing radiation exposure
In order to reduce effects of radiation exposure, there are three main engineering factors that should be considered in general for any radiological application. The factors are time, distance, and shielding as described below[9].
Time
Radiation exposure gets accumulated over time. The longer the exposure time, the more risk of exposure. Therefore, it is mandatory to control time exposure by optimising the radiological procedures. In order to do that, the radiologist should improve his/her skills in interventions such as checking the X-ray at the correct location and at the correct moment with a high resolution image.
Distance
The intensity of the radiation exposure decreases in proportion to the inverse of the distance square. This means that double the distance from the radiation source can reduce the radiation exposure not to 1/2 but to 1/4. Therefore,maintaining standard distance from the X-ray generator is a very effective method for radiation safety.
Shielding
Different materials are used in case of ionising radiation depending on source of radiation. In case of alpha particles, paper can stop radiation, meanwhile, beta particles can be stopped by 1- 2 cm of plastic. Gamma and X-ray photons can be absorbed by lead. In case of neutrons, several feet of concrete are required. Moreover, many shielding devices such as caps, lead glasses, thyroid protectors, lead gloves, and lead aprons are used as Personal Protective Equipment (PPE)[9].
Risk Management in Medical Imaging Devices
According to hazards of medical imaging procedures, medical and engineering staff must identify and mitigate radiation risks to be under control. Proactive procedures, policies, practices, and processes in delivery of diagnostic care should be adopted. Thus, in order to identify risks and mitigate potential harm, the following procedure should be carried out.
1 Identify the hazard with radiological procedures
This includes identification of radiation source, diagnosis protocol, environmental standards, threats, and processes sequence. Additionally, patients, radiologists, visitors, consultants, and vendors should be taken into consideration when hazards are identified. For instance, slip and fall injuries are common risks identified in all environmental settings.
2 Risk assessment
Because risk implies a potential loss, two elements of a risk must be estimated. First, the probability that the risk will become a problem i.e. probability of occurrence. Second, the effect of the risk i.e. consequence or risk severity. Several tools such as hazard/risk analysis, Failure Mode and Effects Analysis (FMEA), and Fault Tree Analysis (FTA) are helpful in risk estimation[10].
3 Risk control
Risk mitigation involves two types of strategies:action planning and contingency planning[10]. Action plan addresses risks that can be mitigated by immediate response, while contingency planning addresses risks that require monitoring for some future response. In both cases, the values of risk metrics must be monitored regularly to monitor impact of control action. In medical imaging devices, action planning is usually adopted.
4 Review control
This is the last step in risk management process. The aim is to assess the risk after control to measure the validity of the action plan in risk mitigation.
Application of Risk Management in Medical Imaging
In this section, principals of risk management are applied on three modalities of medical imaging devices: MRI, CT, and X-rays[11]. Taking into account, review control is avoided.
1 MRI
The MRI is one of the advanced devices that helps to see the tissues and organs inside the human body. One of its advantages is that it does not use radiation but rather imaging using magnetic fields, which makes it safe and harmless as well.
Risk identification: Although MRI does not harm the patient, it does have environmental damage because it is based on a large, stable magnetic field and a variable magnetic field. The strong magnetic field attracts the metal objects, in addition to a loud sound of the device. Moreover, radio frequency energy that is used during an MRI can cause a high temperature. Additionally, the magnetic field may cause burns to patients who haveexternal devicesimplanted.
Risk assessment: Metal objects can lead to damage of the scanner and/or harm patient and medical staff. The sound produced by the MRI may harm the patient’s hearing.
Risk control: Control of the problem of attracting objects to the device due to the magnetic field is carried out by placing the device in a room whose walls and floors are specially designed to resist the magnetic field and that there are devices and tools dedicated to it. A specific distance was determined that cannot be crossed so that the device's magnetic field is not penetrated. As the patient enters the examination, anything metal is removed. To reduce the temperature problem of the device, the device can be operated for a period, then it will be disconnected and completed later to avoid heat.
2 CT
CT scan is a modern device that uses X-rays and works as a scanner to obtain a three-dimensional image of the human body, where it is cut into very thin slices where the doctor can see the bones and some of the organic organs.
Risk identification: Sectional rays are dangerous because the patient is exposed to a large amount of radiation during a short period, which leads to diseases and may recur. If the contrast dye is used, it may lead to an allergic reaction to the dye, which leads to internal injuries. As for the technicians who supervise the cameras, their work is exposed daily to large amounts of radiation, which leads to damage to their organs.
Risk assessment: Exposure of high doses of radiation leading to internal damage of human organs and cells that may cause cancer occurrence.
Risk control: Reducing the number of sessions that the patient is exposed to which in turn will reduce the intake dose. For radiology technicians, they must wear their PPE tools, additionally, specific meals should be provided for them to compensate for any minor damage. Besides, placing the CT device in pre-prepared shielded room with optimal distance from the control room to protect the radiologists and other persons.
3 X-rays
An X-ray is a very common procedure used to take pictures from inside the body. It uses radiation from the X-ray part of the electromagnetic spectrum. They are used to render pictures of limbs, typically to see whether and when there are fractures.
Risk identification: X-rays expose the patient to unwanted radiation, which could potentially cause cancer, although the amount of radiation emitted is minimal. The danger from X-rays comes from the radiation they produce, which may harm living tissue. This risk is relatively small, but it increases with cumulative exposure.
Risk assessment: Exposure of high doses of radiation may lead to internal damage of human organs and cells that may cause cancer occurrence. Moreover, exposure to high radiation standards can result in issues such as loss ofhair, reddening of skin, vomiting, and fainting.
Risk control: Examinations are carried out only when they are required. The safety properties include that X-ray equipment is furnished with incorporate interlocks and shielding. In fact, faulty interlocks may result in unintended exposures. Besides, keeping the optimal distance as a safe barrier is mandatory.
References
[1] C. Lindholm, J.P. Notander, and M. Host, “Software risk analysis in medical device development,”In proceedings of 37th EUROMICRO Conference on Software Engineering and dvanced Applications, 2011.
[2] M.R.Signori, and R. Garcia, “Clinical engineering and risk management in healthcare technological process using architecture framework,” In proceedings of 32nd Annual International Conference of the IEEE EMBS, 2010.
[3] J. Dyro, The Clinical Engineering Handbook, Elsevier Academic Press, Cambridge, MA, USA, 2004.
[4] World Health Organization (WHO), Diagnostic imaging:imaging modalities [Online]. Available:https://www.who.int/diagnostic_imaging/imaging_modalities/en/
[5] S.M.Ghanem, M. AbdelWahed, and N. Saleh, “Automated risk control in medical imaging equipment management using cloud application” Journal of Healthcare Engineering, vol. 2018, pp. 1-8, 2018.
[6] D.R. Dance, et al., Diagostic radiology physics: a handbook for teachers and students, Vienna: International Atomic Energy Agency, 2014.
[7] K.J. Awosan, et al., “Knowledge of radiation hazards, radiation protection practices and clinical profile of health workers in a teaching hospital in northern Nigeria,” Journal of Clinical and Diagnostic Research, vol. 10, no. 8, pp. LC07-LC12, 2016.
[8] M.M. Garau, A.L. Calduch, and E.C. Lopez, “ Radiology of the acute radiation syndrome” Reports of Practical Oncology and Radiotherapy, vol. 16, pp. 123-130, 2011.
[9] J.H. Kim, “Three principles for radiation safety:time, distance, and shielding” The Korean Journal of Pain, vol. 32, no. 3, pp. 145-146, 2018.
[10] P. H. King, R.C. Fries., and A.T. Johnson, Design of biomedical devices and systems. 4th ed., CRC Press, 2018.
[11] MSD Manual Professional Edition, Risks Of Medical Radiation - Special Subjects [Online]. Available https://www.msdmanuals.com/professional/special-subjects/principles-of-radiologic-imaging/risks-of-medical-radiation