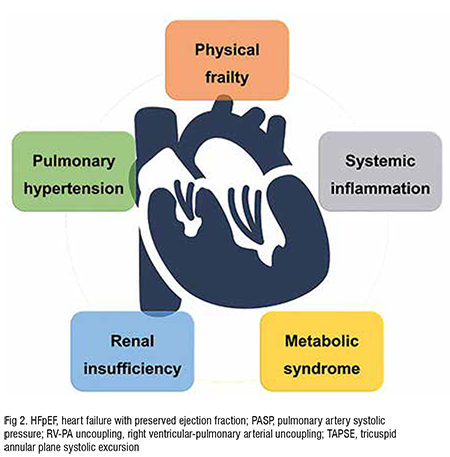
Heart Failure with preserved Ejection Fraction (HFpEF) is a crucial problem among cardiovascular diseases for the lack of established treatment strategies. There must be a need for detailed observational cohort studies for HFpEF patients to elucidate the detailed clinical phenotypes and to find appropriate therapeutic strategies.
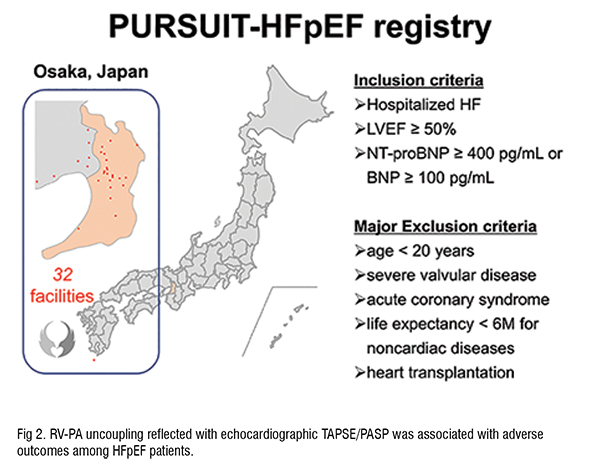
Heart Failure (HF) is a critical social problem all over the world, and HF with preserved Ejection Fraction (HFpEF) has particularly been increasing and upcoming to a bothering issue. Complicated pathophysiology and multiple comorbidities with an aging population makes it rather difficult to find the best way to treat HFpEF patients, and none of specific strategies have been established for the prognostic improvement. In order to understand the characteristics, backgrounds, and underlying problems of current HFpEF patients, we considered detailed observational cohort study must be needed. Based on such a concept, professor Yasushi Sakata (Department of Cardiovascular Medicine, Osaka University Graduate School of Medicine, Japan) launched multi-centre observational cohort study, named PURSUIT-HFpEF registry, from June 2016 to register up to 1,500 HFpEF patients until March 2021. Inclusion criteria were acute decompensated HFpEF diagnosed by the Framingham criteria for HF plus the following: (1) left ventricular ejection fraction ≥ 50 per cent and (2) N-terminal pro-brain natriuretic peptide (NT-proBNP) ≥ 400 pg/mL or brain natriuretic peptide (BNP) ≥ 100 pg/mL on admission. Exclusion criteria were age < 20 years, severe valvular disease, acute coronary syndrome on admission, life expectancy of < 6 months due to prognosis of non-cardiac diseases, and previous heart transplantation.
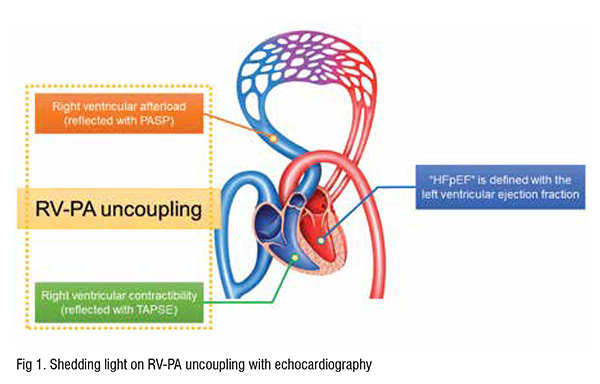
Although Right Ventricular (RV) function had been de-emphasised in the consideration of left-sided HF for many years, it is now evident that RV dysfunction is highly prevalent and resulted in poor prognosis in patients with left-sided HF with HFpEF in the position statement of the Heart Failure Association of the European Society of Cardiology. Even among the parameters related to right heart dysfunction and failure, RV-Pulmonary Artery (PA) coupling has been extensively focused on the prognostic predictability.
Right ventricle is quite sensitive to changes in afterload, and the afterload dependence is even exaggerated in HFpEF patients. Although RV-PA coupling had been evaluated with invasive calculation with Swan-Ganz catheterisation, recent studies have revealed that RV-PA coupling was able to be examined in a non-invasive manner with Tricuspid Annular Plane Systolic Excursion (TAPSE) to Pulmonary Arterial Systolic Pressure (PASP) ratio on echocardiography. TAPSE represents right ventricular contractile function, and PASP is estimated with the pressure gradient of tricuspid regurgitation Doppler wave in addition to the estimated right atrial pressure, presumed with the diameter and inspiratory collapsibility of inferior vena cava. Reduced TAPSE/PASP ratio was associated with worse prognosis in HF (including HFpEF), and a prognostic cut-off value was generally identified as < 0.36 mm/mmHg.
Although treatment strategies were evaluated with randomised clinical trials, there were unavoidable discrepancies between trial candidates and realworld patients. The clinical impact on HFpEF patients of Angiotensin II Receptor Blockers (ARBs) of irbesartan and candesartan had been evaluated with I-PRESERVE (n = 4,133) and CHARM-Preserved (n = 3,023) trials, which had been unfortunately failed in establishing desirable evidence of ARB on HFpEF patients. While the mean age of HFpEF patients reported from a large size of observational study of the heart failure component of Get with the Guideline (GWTG-HF) registry (n = 18,299, between 2005 and 2009) was as high as 82 years, the candidate ages of I-PRESERVE (mean of 72 years, age ≥ 75 years was 34 per cent) and CHARM-Preserved (mean of 67 years, age ≥ 75 years was 27 per cent) were quite different. Considering these discrepancies, we should reassume the pathophysiology and treatment strategy for HFpEF patients based on real-world data.
As described above, the prognostic importance of RV-PA coupling for HFpEF patients had been established, however, the prognostic importance of TAPSE/PASP < 0.36 mm/mmHg was proved based on HFpEF populations haemodynamically validated with right heart catheterisation, which is ethically inappropriate for HFpEF patients in general. In order to verify the clinical prognostic usability of TAPSE/PASP ratio, investigations based on widely included HFpEF patients should be needed.
From our multi-centre prospective observational study, we examined the prognostic importance of TAPSE/PASP ratio among 655 hospitalised HFpEF patients. The median age was as high as 83 years, which was comparable to the patient characteristics of the large cohort of GWTG-HF registry. We should state the patient characteristics of this cohort that 56 per cent were females, median body mass index was as small as 21.2 kg/m2, atrial fibrillation coexisted as much as 40 per cent, and the median NT-proBNP level was 1,080 pg/mL. The median value of TAPSE/PASP at discharge was as high as 0.54 mm/mmHg, and the ideal cutoff value of predicting adverse outcomes, defined as a composite of all-cause death, HF re-admission, or cerebrovascular events, was also as high as 0.48 mm/mmHg (area under the curve of receiver operating curve analysis = 0.59, P< 0.0001).
Kaplan Meier curve analyses showed that TAPSE/PASP < 0.48 mm/ mmHg was sufficient to predict the poor outcome (Log-rank P< 0.0001 for composite endpoint), and multivariable Cox regression testing revealed that TAPSE/PASP <0.48 mm/mmHg was significantly associated with the composite endpoint independently from multiple covariates including age, female sex, atrial fibrillation, renal dysfunction, and NT-proBNP elevation (hazard ratio = 1.77, 95 per cent confidence interval; 1.34-2.32, P< 0.0001). As a matter of course, a lower generally accepted threshold of TAPSE/PASP< 0.36 mm/mmHg was also able to predict the poor outcome; a higher threshold of 0.48 mm/mmHg was proved to be sufficient for the prognostic prediction in this cohort. There must be racial differences between Asians and Westerners which made the different meanings of TAPSE/PASP ratio, however, the evidence derived from our registry should reflect the precise characteristics of the realworld HFpEF patients.
Although major pathophysiology among HF and the definition of the ejection fraction as HFpEF are derived from the left side of the heart, our findings suggested that RV-PA uncoupling, deeply related to the right side of the heart, observed in echocardiography had a crucial prognostic meaning even among elderly multiple comorbid HFpEF patients.
Findings from the PURSUIT-HFpEF registry suggest the necessity of a treatment strategy for HFpEF patients based on RV function and pulmonary circulation. For instance, the short term beneficial effects of -adrenergic agonists for HFpEF have been considered from such a viewpoint. Andersen et al. reported that dobutamine infusion caused greater pulmonary vasodilatation with enhanced reductions in PA resistance, greater increase in PA compliance, and a more negative slope in the PA pressureflow relationship in a prospective trial in HFpEF patients. Following this study, in a randomised, double-blind, placebocontrolled trial for HFpEF patients, Reddy et al. described the beneficial effects of an inhaled -adrenergic stimulant that improved the primary endpoint of exercise pulmonary vascular resistance. Both trials showed that beneficial effects on acute improvement were achieved with the improvement of RV-PA uncoupling with -adrenergic stimulation.
The abilities of these and other potential therapeutic agents for HFpEF patients to improve RV-PA uncoupling, and ultimately the prognosis are needed to be explored in further investigations.
References:
1. S Suna et.al. Study protocol for the PURSUIT-HFpEF study: a Prospective, Multicenter, Observational Study of Patients with Heart Failure with Preserved Ejection Fraction, BMJ Open 2020;10:e038294.
2. TM Gorter et.al. Rightheart dysfunction and failure in heart failure with preserved ejection fraction:mechanisms and management. Position statement on behalf of theHeart Failure Association of the European Society of Cardiology. Eur JHeart Fail. 2018;20:16–37.
3. A Nakagawa et.al. Prognostic Importance of Right Ventricular-Vascular Uncoupling in Acute Decompensated Heart Failure With Preserved Ejection Fraction, Circ Cardiovasc Imaging. 2020;13:e011430.
4. MJ Andersen MJ et al. Enhanced pulmonary vasodilator reserve and abnormal right ventricular: pulmonary artery coupling in heart failure with preserved ejection fraction. Circulation Heart failure 2015;8:542-50.
5. YNV Reddy et al. The β-Adrenergic Agonist Albuterol Improves Pulmonary Vascular Reserve in Heart Failure With Preserved Ejection Fraction. Circulation research 2019;124:306-314.