The environment within the hospital is critical for life support. Environmental concerns affect the hospital internally and externally. Indeed, the hospital requires a safe internal environment. Externally the hospital is a contributor to the environmental load of the community. Some internal factors that impact upon hospital environment safety are presented.
Hospitals are representative of complex environment in which different aspects including patients, staff, equipment, services, and information are interfaced. Maintaining a safe environment reflects a level of competent healthcare that must be fulfilled for patient safety. In this context, the clinical engineer plays an important role in providing safe environment within hospital. In general, many factors affect hospital environment internally and externally. Many internal factors have a significant impact on hospital environment such as waste management, noise, and infection control; and external factors such as sources and treatment of water, sewage treatment and disposal. In this article, some of internal factors are discussed:
1. Waste management
2. Noise
3. Infection control
4. Radiation safety
5. General building safety
6. Water quality
7. Heating, Ventilation, and Air Conditioning
Waste management is crucial to promote high quality of healthcare and safe environment within hospitals. Medical waste is any waste occurring as a result of medical services and scientific research in medicine. In general, the amount of waste generated by healthcare activities is 80 per cent general waste and the remaining 20 per cent is hazardous material. World Health Organization (WHO) divides medical waste into seven basic categories based on their properties and risk level:
• Infectious waste
• Pathological waste
• Sharps
• Chemicals
• Pharmaceuticals
• Genotoxic waste
• Radioactive waste

The most important factors that should be considered in waste management systems are
• Collection system in the generation site (i.e. segregation system, type of containers/bags)
• Time and temperature of temporary storage (generation side)
• Transport requirements
• Central storage conditions
• Approved disposal method
Every factor should be taken into consideration for a proper waste management system. For example, in collection system medical staff that is responsible of segregation stage must follow the guidelines approved by Ministry of Health (MOH) of their county. For central storage area it should not be located near the general waste central storage. Further more, waste disposal process must be carried out according to approved method such as incineration which is requiredfor disposal of pathological specimens. The summary of approved disposal methods based on the class is presented in Figure. 1
Noise is defined as unwanted sound. Several studies have been conducted for hospital noise that linked hospital noise to a variety of negative physiological outcomes. The WHO has recommended that noise level should not exceed 35 dB in rooms where patients are treated or observed and 30 dB in wards rooms. In 1974, the US Environmental Protection Agency (EPA) suggested that the peak noise level in a hospital should not exceed 45dB during the day and 35 dB at night. In fact, the noise level is hospitals usually more than the recommended levels.
Hospitals have various sources of noise such as alarms, paging systems, telephones, computer printers, televisions, delivery carts, staff conversation, equipment, housekeeping activities, air conditioning systems, doors opening and closing, and sounding systems. Of course, one physical effect of the noise is human stress which should be avoided in hospital environment. Topf and Dillon (1988) have described human effects due to noise-induced stress as decrease in sustained attention, rapid detection, multiple single tasks, and incidental memory.
To overcome the problem of noise within hospitals, some preventive procedures should be carried out. One form is to measure the noise level periodically to reduce patient exposures to such noises. Another approach is to perform a regular check and maintenance to all systems that are considered as sources of noise including equipment. Also some practices could reduce noise level, these include: handling different alarms, obligation of instructions in critical areas such as intensive care units, making clear circulation paths for patients and staff, and well training for services providers such as housekeeping.

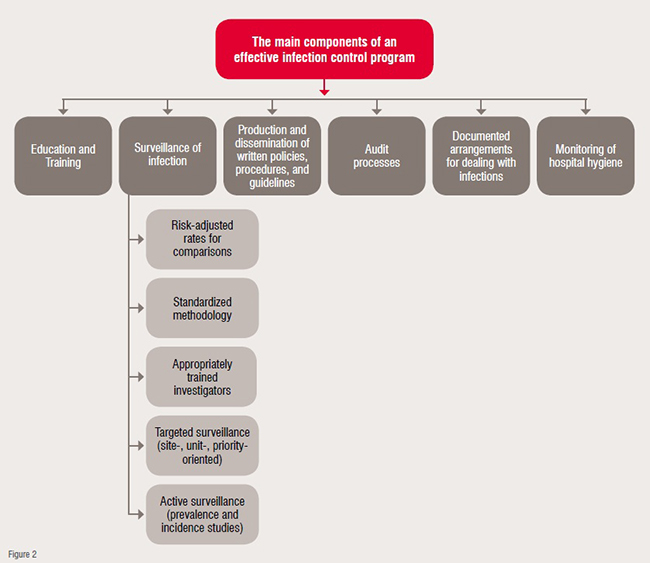
Infection control provides a framework for identification of a hazard and development of an action plan to eliminate the hazard or minimise its effect through control measures. Control has been achieved by recognising the means of growth, reproduction and transmission of pathogenic microorganisms. The main components of an effective infection control program are illustrated in Figure 2 and listed as following:
• Education and training
• Surveillance of infection
• Policies, procedures, and guidelines
• Audit processes
• Documented arrangements
• Monitoring of hospital hygiene
The WHO has classified infection control practices into two main categories: standard precautions and additional (transmission-based) precautions. These category items are Standard precautions include the following items
• Hand washing and antisepsis (hand hygiene)
• Use of personnel protective equipment when handling blood, body substances, and secretions
• Appropriate handling of patient care equipment and soiled linen
• Prevention of needlestick / sharp injuries
• Environmental cleaning and spills-management
• Appropriate handling of waste
Additional (transmission-based) precautions while ensuring standard precautions include
• Airborne precautions
• Droplet precautions
• Contact precautions
For infection control management, existence of a clear written policy within the facility to closely monitor and implement infection control processes with feedback measurement as well as compliance with infection control practices is essential. Moreover, routine practices such as aseptic techniques, single-devices, reprocessing of instruments and equipment, antibiotic usage, handling and use blood and blood products as well as environmental management practices is fundamental for this issue.
The last two decades have witnessed a technological revolution in diagnostic and therapeutic medical imaging. However, minimising the risk of radiation exposure is still a challenge. According to a 2010 US Food & Drug Administration (FDA) white paper, per capita exposure to ionising radiation (from all sources) increased from 3.6 mSv (milli Sievert) in 1980 to 6.25 mSv in 2006. During this time, the contribution that was attributable to medical imaging increased from 15 per cent in 1980 to 48 per cent in 2006, and over two- thirds of all medical imaging in 2010 involved ionising radiation.

Radiation protection is a public health issue for a number of reasons. First, health effects of radiation are not unique. Second, individuals have only a limited ability to structure or control their own environment. Although radiation exposure awareness has increased among the general public, there is still very little monitoring of cumulative radiation exposure over a patient's lifetime. Successful radiation safety progrmmes must balance engineered safety and personnel training considering technical, scientific, economic, human, and ethical aspects of radiation use. The medical safety progrmme must adequately protect patients, care givers, visitors, and the general public. To minimise external radiation exposure hazards in ionising radiation, fundamental principles in radiation protection should be identified as follow:
1. Existence of radiation safety program that cover and support the following activities
• Regulatory activities related to radioactive material license
• Multilevel relation safety training
• Monitoring of occupational radiation doses of personnel
• Control of radioactive materials
• Active participation in planning of new or remodeled facilities
• Response and investigation of incidents/accidents
• Quality management program.
2. Time, distance, and shielding are other crucial elements in radiation safety that should be regarded.
Time: The simplest method for protection from ionising radiation is to spend as little as possible in the vicinity of radiation source, in addition, reducing the exposure time by one half reduces the dose received by one half
Distance: Doubling the distance between the person and the source helps to reduce the exposure to a quarter of its original value
Shielding: Shielding is considered as the most significant line of defense. The more mass that is placed between a source and a person, the less radiation the person will receive. Gamma ray can be attenuated by using lead shields or concrete.
Nonionising radiation is a significant health hazard in all hospitals. This type includes ultraviolet, microwave, and laser radiation. Ultraviolet (UV) radiation is frequently used in sterilisation procedures. In fact, UV exposures are best controlled by limiting exposures as function of energy. In application, Microwave radiation is commonly used in hospital diathermy treatment and in microwave ovens. Microwave radiation is controlled by limiting exposure and sources should be periodically surveyed with measurement equipment. On the other side, Lasers have an increasing role in medical treatment. Eyewear is the most common method of protection.
Safety of building is the practice of designing, constructing, operating, maintaining, and removing buildings in ways that gives no one deteriorated health, injuries or death due to the use of building. The vast investment in health infrastructure-hospitals can absorb up to 70 per cent of ministry of health budgets-can be lost when poorly constructed hospitals are destroyed or damaged. Hospitals can be made more resilient and functional through action to improve the sustainability of health infrastructure, including measures to increase the reliability of power and water supply systems.
The physical structure of the hospital may pose hazards to the patients and workers alike. The most common causes of compensable work injuries are manual material handling, falls, and getting struck by falling or moving objects. Accidents and injuries due to falls and collision can be minimised through:
• Establishing a traffic flow pattern
• Ensuring clean, dry, unobstructed, and slip-resistant surfaces
• Maintaining railings and stair surfaces in good condition
• Supervising patients to minimise unnecessary trave.
Fire and smoke alarm system is considered a means to ensure life safety as well as building safety. Hospitals must comply with the life safety code NFPA 101 of the National Fire Protection Association, published in 1997. This standard provides detailed specifications for design, construction, and operation of building to protect occupants from fire.

Gases cylinders and distribution systems are usually considered an integral part of the hospital structure. Medical gases are vital elements in patient treatment as well as laboratory procedures. Most hospitals have a permanently installed gas distribution system. In this system gas cylinders may be stored in a centralised location separate and apart from other hospital functions. Any gas cylinder should be accorded the following elements of care:
• Identify cylinders by written name and colour coding
• Secure cylinders to wall or within enclosures
• Cap all cylinders not in immediate use
• Protect cylinders from temperature extremes
• Never use oil or grease on oxygen or nitrous oxide equipment
• Never permit smoking or use flames near oxygen or nitrous oxide equipment
Check gas regulators and do not use a regulator for oxygen or nitrous oxide after it has been used with any other gas.
Water is a strategic energy resource that should be used and managed properly. In hospitals, water is a necessary utility which is obtained from outside sources. This utility may serve as a medium for the spread of infections from outside sources to the hospital. A complete chemical analysis of water is required to establish quality levels. This analysis may be performed by local public health agencies or by hospital staff. If the hospital has storage water tanks, they should be cleaned regularly and the quality of water should be sampled periodically to check for bacterial contamination.
In healthcare facilities, the demand of water by different services and users depends on many issues but must always consider potential risks and negative impacts of water use by people (e.g., infection) and equipment (e.g., fast deterioration and damage); the collection and treatment prior to its final disposal and discharge into the sewer system, and the possible environment impact upon the water use cycle (e.g., contamination).
Once the water is delivered to the hospital, it requires further treatment and conditioning to meet specific needs. The typical treatment of the hospital water supply includes deionisation, distillation, and sterilisation. Most healthcare facilities have six major areas of water consumption: sanitation, Heating, Ventilation, and Air Conditioning (HVAC), clinical and medical procedures, laundry, food services, and miscellaneous uses. Sanitation and HVAC consume approximately 60 percent of the water in most facilities.
Waste water collected from different services within hospital carries a variety of chemicals and biological pollutants, several of which are hazardous. Wastewater should be included in a hospital's water management and it should be closely monitored and pretreated prior to discharge into the public sewer system.
The purpose of HVAC system is to provide and maintain environmental conditions, including proper airflow, heating, and cooling within a certain area or the entire hospital. Installation of HVAC is one of the most important factors by which the architect can combat bacterial infection, and at the same time create environmental comfort.
HVAC system is designed to meet specific values of temperature, relative humidity, and air changes frequency within different areas in hospital based on standards of design. For example, high risk areas such as operating rooms and intensive care units require special ventilation systems through filtration systems (e.g., HEPA filters) and pressure relationship to adjacent areas. In general, clean atmosphere reduces the risk of airborne infection, and dangerous of gases explosion.
References:
01. Rolewicz-KalinskaA. Logistic constraints as a part of a sustainable medical waste management system. Green Cities – Green Logistics for Greener Cities, 2 nd, Szczein, Poland, 2016; pp. 473-482.
02. Oli AN, Ekejindu CC, Adje DU, Ezeobi I, Ejiofor OS, Ibeh CC, Ubajaka CF. Healthcare waste management in selected government and private hospitals in Southeast Nigeria. Asian Pac J Trop Biomed. 2016; 6(1):84-89.
03. Emmanuel J, Chartier Y, Pieper U, Prüss A, Rushbrook P, Stringer R, Townend W, Wilburn S, Zghondi R. Safe management ofwastes from health-care activities. 2nd edition, World Health Organization,2014.Available at:http://www.searo.who.int/srilanka/documents/safe_management_of_wastes_from_healthcare_activities.pdf?ua=1
04. Hamadan N, Sabri M, Mohammed AH, Awang M, AbdRahman MS, Rosli NW, NikLah, NMI. The implementation of clinical waste handling in Hospital SultanahAminah Johor Bahru (HSAJB).International Congress on Interdisciplinary Business and Social Science, 2012; pp. 802-807.
05. World Health Organization. Practical guideline for infection control in healthcare facilities. 2004. Available at http://www.wpro.who.int/publications/docs/practical_guidelines_infection_control.pdf
06. Cunha M, Silva N. Hospital noise and patients wellbeing. Social and Behavioral Sciences. 2015. 171: 246-251.
07. Ulrich R, Quan X, Zimring C, Joseph A, Choudhary R. The role of the physical environment in the hospital ofthe 21st century:Aonce-in-a-lifetime opportunity. 2004. Available at https://www.healthdesign.org/system/files/Ulrich_Role%20of%20Physical_2004.pdf
08. Mamishi S, Pourakbari B, TeymuriM, Babamahmoodi A, Mahmoudi S. Management of hospital infection control in Iran: A need for implementation multidisciplinary approach. Osong Public Health Res Perspect. 2014; 5(4):179-186.
09. Mastracci TM. Radiation safety: A call to arms. Eur J VascEndovasc Surg. 2015; 50:1-2.
10. Dyro J. Clinical engineering handbook. Elsevier press, 2004.
11. Indian Institute of Technology Bombay. Radiation safety. Available at
http://www.iitb.ac.in/safety/sites/default/files/Radiation%20Safety_0_0.pdf
12. World Health Organization. Comprehensive safe hospital. 2015. Available at http://www.who.int/hac/techguidance/comprehensive_safe_hospital_framework.pdf
13. Medical gas pipeline systems – British compressed gases. Available at http://www.bcga.co.uk/assets/HTM_02-01_Part_A.pdf
14. Heating, ventilation, and air conditioning (HVAC) systems: energy-efficient usage and technologies. Available at
http://www.eskom.co.za/sites/idm/Documents/AdvisoryServicesHVACSystemBrochure.pdf
15. McDowall R. Fundamentals of HVAC systems. Academic press. 2007.