This article explores the importance of a multidisciplinary approach to cancer care and the current obstacles of accessing radiation oncology including: current consumer and clinician perceptions, infrastructure challenges constructing radiation oncology facilities across ASEAN, and regional shortages of specialised clinical expertise. It also discusses future trends – increase use of AI, and remote clinical and training capabilities.
In 2020, there were an estimated 19.8 million new cancer cases and over 10 million reported cancer deaths1. By 2040, the number of new cancer diagnoses is expected to rise by 29.5 million annually and will continue to be one of the leading causes of death worldwide2. Long-term effects of COVID-19 will exacerbate the cancer burden and a widening global healthcare gap is creating unending roadblocks to vital cancer treatment. How can we overcome barriers to care and what investments need to be made to take us into a future less burdened?
The first phase in solving any problem is acknowledging it. In 2050, in Asia-Pacific alone a staggering 9.8 million new cancer cases are projected, a number that will place unsustainable pressure on public hospitals and all available local cancer treatment facilities3. Lack of access to cancer care needs to be resolved and more importantly access to comprehensive cancer care is required. Radiation therapy is an effective and proven modality for treating a wide-range of cancers, with over 50 per cent of new cancer cases clinically indicating the patient should receive radiation therapy over the course of their treatment4. Radiation therapy is also a well-tolerated and highly effective treatment in palliative cases and results in higher quality of life. However, across Asia and many developing countries radiation therapy is being under-utilised due to several industry, community, and economic factors.
From conversations with our oncologists in Singapore it is clear there continues to be some misconceptions around the safety and efficacy of radiation therapy among general community, particularly those in older generations. Similarly, a few years ago there was less knowledge of radiation oncology even within the clinical setting, where referral pathways would often bypass a Radiation Oncologist. While today, Singapore does enjoy exceptional healthcare and there is a greater emphasis on multidisciplinary meetings and a much higher uptake of radiation referrals and general community awareness, there is still room to grow in education and utilisation. However, in surrounding countries like Vietnam, Indonesia, Laos, and regional areas of Malaysia misconceptions of radiation therapy prevail with fears of safety, myths around side effects, and a lack of radiation oncology referrals affecting the regions cancer mortality rates. Investing in education programmes and support and advocacy groups is an important step to eliminating these perceptions and empower patients and doctors to make informed decisions.

Radiation oncology facilities require substantial financial investment and infrastructure. On average, low to middle income countries (LMICs) have access to only 0.71 radiation therapy machines per million population in comparison to 7.62 machines per million in high income countries5. This gap will accelerate in correlation with expected increased cancer diagnoses, so what is the solution?
Successful healthcare ecosystems thrive on partnerships and collaborations. The industry should be seeking greater investment in government and private sector partnerships in order to close the infrastructure gap, increase efficiencies and foster multidisciplinary advancements in cancer treatment. For LMICs in particular, it’s also important to establish national cancer control programmes and increase discussions with international bodies such as the World Health Organization (WHO) and the Union for International Cancer Control (UICC) to improve patient access. This multi-sectoral approach will allow countries to close local knowledge gaps and build more facilities where they are needed. But establishing radiation oncology departments doesn’t just involve bricks and mortar, specialised technical support and clinical expertise is required.
In a survey by the Federation of Asian Organizations for Radiation Oncology, member countries saw only 54 per cent of the region's need for radiation oncologists being fulfilled, with most countries in the region producing less than 10 new radiation oncologists annually6. This shortage runs across all radiation professionals, including medical physicists, radiation therapists and specialised oncology nurses. The lack of expertise and bottlenecks in training causes lower quality of care, an inability to introduce new treatment technologies, issues with machine maintenance, and ultimately poorer patient outcomes. So if we can’t access local expertise, how can we bring the best possible care to more people?
At Icon, we are proud to have longstanding relationships with shared care partners across the ASEAN region which enables us to deliver seamless care both travelling into Singapore for treatment and follow-up care within the patient’s own country. This shared-care model utilises Singapore’s well-experienced oncologists and clinical teams, alongside hospitals across ASEAN to help eliminate deficiencies of expertise. During COVID-19, this model evolved with the increase use of telehealth and safe home delivery of medications to dissolve geographical barriers and continue access to treatment.
Similarly, whilst there has been an increase of medical physicists in the region, the majority of training practices have not changed over the last six to ten years7. In that time the complexity of radiation technology has increased significantly causing a knowledge shortfall in local physicists. In 2019, Icon established a partnership with Vinmec Central Park International Hospital in Ho Chi Minh City, Vietnam to manage a new radiation oncology department onsite. This centre was only made possible with the support of Icon’s internationally recognised medical physics team who worked alongside local teams to commission the linear accelerator and provide ongoing training for machine maintenance and deployment of new techniques. However, to create sustainable healthcare, robust training programmes should be implemented.

‘Give a man a fish he’ll eat for a day, teach a man to fish he’ll eat for a lifetime.’ Whilst there is no one true silver bullet to closing the radiation oncology care gap, investment in education is a sure fire way to improving outcomes and sustainable growth of radiation therapy.
Striving to improve health outcomes across ASEAN, Icon Group recently launched Icon ECHO clinics, utilising the Project ECHOTM (Extension for Community Healthcare Outcomes) model. Project ECHO uses technology to share knowledge across miles, leveraging free web-based platforms to connect clinicians with real-time collaborative, case-based learning. Icon ECHO clinics are based in Singapore and utilise the group’s international network of clinicians to support practitioners across the Asia Pacific empowering them to deliver better care to people within their communities. In its early stages, these clinics have seen positive outcomes and have nurtured existing shared care partnerships. The clinics continue to evolve and can easily be adapted to various clinical streams and disciplines. It is proof that collaboration and knowledge is key to the creation of healthy communities.
Icon has partnered with Mt Alvernia Hospital in Singapore to establish a state-of-the-art cancer centre on the Mt Alvernia hospital campus which will bring all aspects of cancer care under the one roof. Not only will this centre contribute to the need for increased access to comprehensive care, it will also elevate the standard of clinical knowledge as the home to Varian’s regional training hub. The training facility will service radiation oncologists, medical physicists and radiation therapists across South- East Asia and foster a learning culture, providing clinical education and training to upskill medical professionals across ASEAN. This builds on Icon’s longstanding global partnership with Varian which allows for economies of scale, early adopters of new and emerging radiation technologies and products, and a collaborative workforce which allows Icon’s clinical experts to contribute to advancing Varian’s innovations through international consortiums, committees and large-scale research projects.
Increased utilisation of remote technologies also paints much of this training solution and form a large part of the future of radiation therapy.
With defined cancer care roadblocks and the progression of solutions, we have the power to forge a better way forward. Research and trends in cancer care indicate the acceleration of radiation therapy techniques and investment in emerging technologies are and will lead to better patient outcomes.
COVID-19 expedited the need for healthcare to innovate. At Icon we quickly evolved our international remote capabilities, which are underpinned by a centralised team of expert dosimetrists and radiation therapists. Already operating a well-established remote radiation therapy planning function, which sees this central team plan personalised complex treatment plans for patients in China and the broader Icon network, we took this expertise a step further. Investing in assisted reality (AR) headsets, Icon has introduced a remote radiation therapy training program where our international teams remotely train new clinical teams in China, Australia and New Zealand, with AR headsets that allow both trainer and trainee to walk through and assess processes in real time. This has eliminated geographical barriers and is elevating the standard of local expertise, which can be seamlessly deployed anywhere in the world. It’s these technological innovations that are shaping the future of radiation therapy.
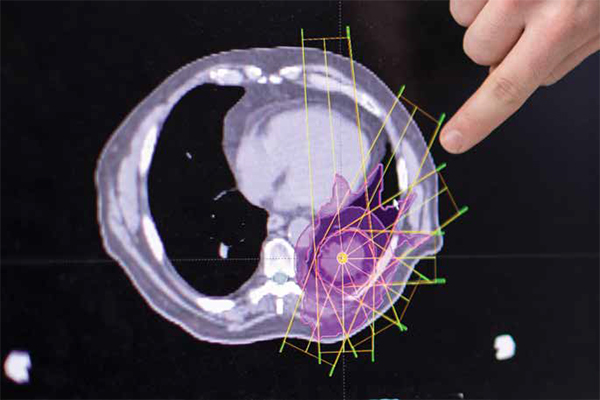
Patients diagnosed with multiple brain metastases are continuously seeing better quality of life through new evolutions in stereotactic radiosurgery. This technology is eliminating the severe side effects and often poor outcomes of whole brain radiation, allowing clinicians to precisely target multiple tumours in the brain. Today, with this cutting-edge technology radiation oncologists are targeting as many as 20 metastases in one treatment plan and are continuing to see an increase in the total volume of tumour which can be treated at any one time, giving new hope to thousands of palliative patients. Similarly there have been evolutions in Image Guided Radiation Therapy, Proton therapy and this concept of flash therapy, treating the entire dose of radiation at once in one large precise fraction, rather than over the traditional daily fractions8. Most recently, the use of artificial intelligence (AI) is allowing oncologists to adapt, replan and optimise radiation delivery in real-time accounting for daily changes in tumour shape and normal organ movements. This use of AI based algorithms is revolutionising precision radiation both during treatment and even during the planning stages9.
The field of radiation oncology will continue to thrive in a tech-focused future. The promising use of theranostics is seeing the implementation of radioactive drugs to identify tumours and deliver therapy directly in the tumour cells, limiting damage to surrounding healthy tissue and organs. The use of AI is in its infancy, but medical physicists and engineers are continuing to see benefits across industries and apply these within radiation technology. The machines are getting smarter, and clinicians are pushing the limits alongside these growing developments.
The future does look bright but if we are to affect change, decrease cancer mortality and increase access to comprehensive care we need to invest in sustainable solutions. The healthcare industry must consider the needs of specific countries, continue to crosscollaborate, place cancer on the agenda, educate and eliminate barrier through innovation. Only then can we have a future less burdened by cancer.
References:
1. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 30 Cancers in 185 Countries. Published in CA: A Cancer Journal for Clinicians Volume 71, Issue 31, May/June 2021 Pages 209-249. https://acsjournals.onlinelibrary.wiley.com/doi/full/10.3322/caac.21660
2. International Agency for Research on Cancer. WHO Global Cancer Observatory [website] https://gco.iarc.fr/ (accessed 4 October 2021)
3. Cancer Burden and Trends in the Asia Pacific Rim Region. Published in Asian Pac J. Cancer Prev. 2005 Apr – Jun; 5(2) pg 96-117. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4170690/
4. Delaney G, Jacob S, Featherstone C, et al. The role of radiotherapy in cancer treatment: Estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer. 2005;104:1129–1137.
5. Radiation Therapy Infrastructure and Human Resources in Low- and Middle-Income Countries: Present Status and Projections for 2020. International Journal of Radiation Oncology 2014 (Vol 89. 3). http://www.sdradiation.com/press-releases/RT-Infrastructure-Resources-low-and-middle-income-countries-Projections-for-2020.pdf
6. Global Radiotherapy: Current Status and Future Directions – White Paper. DOI: 10.1200/GO.21.00029 JCO Global Oncology no. 7 (2021) 827-842. Published online June 8, 2021. https://ascopubs.org/doi/full/10.1200/GO.21.00029
7. Surveying trends in radiation oncology medical physics in the Asia Pacific Region. European Journal of Medical Physics (June 16, 2016). https://www.physicamedica.com/article/S1120-1797(16)30114-4/fulltext
8. Flash radiotherapy: history and future. Frontiers in Oncology 25 May 2021. https://www.frontiersin.org/articles/10.3389/fonc.2021.644400/full
9. The Emergence of Artificial Intelligence within Radiation Oncology Treatment Planning. Oncology 2021;99:124-134. doi: 10.1159/000512172 https://www.karger.com/Article/FullText/512172