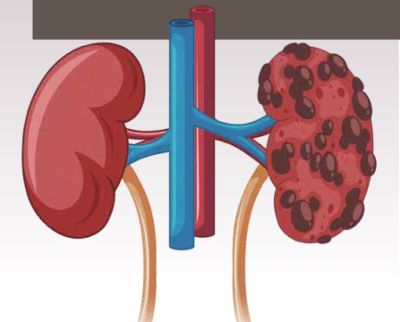
Diabetes is the cause of multiple complications, including cardiovascular, retinopathy, and chronic kidney disease (CKD). CKD, in diabetics, in particular, presents a complex spectrum as it encompasses both classical diabetic kidney disease (DKD), non-diabetic kidney disease (NDKD), and a combination of both. This article aims to briefly elucidate the epidemiology and pathology of both DKD and NDKD.
Triggered primarily by lifestyle changes, diabetes is assuming menacing proportions. According to reports from IDF Diabetes Atlas-2021, 1 in 10 people worldwide suffers from diabetes. That translates to 537 million patients, of which 95 per cent are of Type 2 (T2DM). The predicted trajectory of progression is 643 million by 2030 and 783 million by 2045. It is debated that SARSCoV- 2 infection may have led to the appearance of multiple de novo T2DM cases. The hallmark of diabetes is dysregulated glucose metabolism, either due to the malfunctioning of insulinproducing pancreatic beta cells or due to the inefficiency of the body to use insulin, leading to high blood glucose levels. High blood sugar leads to severe complications, including hypertension, diabetic retinopathy (DR), cardiovascular diseases, and CKD, to name a few! CKD is described as a time dependent progressive loss of kidney function. The spike in CKD observed over the last few decades has been attributed to the increasing cases of diabetes. Between 1990 and 2017, the world witnessed a rise of 9.5 per cent in CKD cases, and in the same time frame, the incidence of global diabetes grew from 11.3 million to 22.9 million cases, a rise of more than 100 per cent. It is projected that nearly 50 per cent of all T2DM patients and over 33 per cent patients with type 1 diabetes (T1DM) will develop CKD. Although CKD can also occur in non-diabetics, the spectrum of CKD in people with diabetes is particularly complex.
Regardless of disease etiology, the existing clinical classification of CKD is centered on the estimated glomerular filtration rate (eGFR) and albumin: creatinine ratio (ACR). Patients are stratified based on eGFR values as G1-G5 (G1 ≥90, G2=60-89, G3a= 45-59, G3b = 30-44, G4= 15-29, G5 <15), and on the ACR as A1-A3 (A1 <30, A2= 30-300 and A3 >300). G1 represents normal or high eGFR, whereas G5 represents kidney failure. On the ACR scale, A1 represents normal, whereas A3 represents severely increased albuminuria. This has greatly broadened the horizon of clinical presentations for diabetic kidney disease (DKD), identifying a distinct class of patients displaying the phenotype of non-albuminuric CKD. The term diabetic nephropathy (DN) is applicable for patients presenting persistent clinically detectable proteinuria, tandemly elevated blood pressure, and a concomitant decline in eGFR. Structural changes in the renal system are a signature profile in DN observed in kidney biopsies, both in T1DM and T2DM. However, the presence of predominant vasculopathy, interstitial fibrosis, tubular atrophy, and/or specific glomerular changes or near-normal renal structure has also been reported in biopsies obtained from patients with T2DM. This may be independent of eGFR, albuminuria status, or any other renal function parameter. Such cases are termed non-diabetic kidney disease (NDKD). To make matters complex, cases have been reported where NDKD may occur alone or superimposed with DN presentations!
DKD was initially described by Mogensen et al. in 1983 as a progressive disease that began with the loss of small amounts of albumin into the urine (30–300 mg per day), termed microalbuminuria or occult or incipient nephropathy. As the amounts of albumin continue to rise in urine and are detectable by traditional dipstick (>300 mg per day), then it is termed macroalbuminuria (proteinuria) or overt nephropathy. This transition may occur over a period of 10-15 years. End-stage renal disease (ESRD) is manifested in 50 per cent of T1DM patients with overt proteinuria within ten years and in >75 per cent by 20 years. Since T2DM is more often associated with late detection, a larger percentage of T2DM patients present established proteinuria at the time of diagnosis. Without definite clinical intervention, up to 40 per cent of T2DM patients with microalbuminuria progress to overt nephropathy. Statistically, only 20 per cent of the patients with overt nephropathy were found to progress to ESRD within 20 years of onset.
Class 1: Mild or non-specific light microscopy changes and electron microscopy–proven glomerular basement membrane (GBM) thickening.
Class 2a: Mesangial expansion, mild.
Class 2b: Mesangial expansion, severe.
Class 3: Nodular sclerosis (Kimmelstiel–Wilson lesion) and
Class 4: Advanced diabetic glomerulosclerosis (scarring).
The predominant type of lesion observed in patients displaying T1DM and DN is nodular glomerulosclerosis. Other common lesions include hyalinosis of afferent and efferent arterioles, glomerular capsular drops, diffuse glomerular lesions with capillary wall thickening, and mesangial matrix expansion.
An atypical DKD phenotype characterised with low eGFR, but no microalbuminuria has been reported. This is termed normoalbuminuric CKD; nearly 25 per cent of diabetic patients are said to present this condition. On a structural aspect, glomerular or non-glomerular renal changes in T2DM are more heterogenous in normoalbuminuric than in albuminuric renal insufficiency. Research suggests uncontrolled hypertension may be the most important predictor for people with diabetes developing CKD (Source: National Kidney Foundation). Specific high blood pressure medications such as angiotensin-converting enzyme (ACE) inhibitors and the angiotensin-2 receptor blockers (ARBs) blocking the reninangiotensin-aldosterone system (RAAS) pathway may be the most effective in preventing DKD. It is, hence, important for people with diabetes to keep their blood pressure under check.

In patients with diabetes, NDKD can also occur. NDKD can be either alone or superimposed with DKD. Glomerular causes of NDKD include membranous nephropathy, immunoglobulin A (IgA) nephropathy, hypertensive renal disease, glomerulonephritis, acute interstitial nephritis (AIN), focal segmental glomerulosclerosis (FSGS) and glomerulonephritis due to ANCAassociated disease and anti-GBM glomerulonephritis.
The diagnosis of NDKD in diabetic patients is complicated by the overlapping histological findings of the mild glomerulonephritis associated with initial DKD changes. NDKD might also appear similar to Class I DN. Electron microscopy can be a valuable tool in assessing renal biopsy samples for the discrimination of NDKD. Various clinical predictors have been proposed to distinguish between NDKD and DKD. The presence of DR is strongly correlated with DKD. However, it is reported that up to 70 per cent of diabetic patients with no retinopathy can present albuminuria and concomitant DKD. This suggests that while DR is an essential tool to indicate either NDKD or DKD, it cannot be an absolute exclusion criterion. The onset time of diabetes is also helpful in distinguishing between NDKD and DKD. It is generally accepted that T2DM less than five years is strongly suggestive of NDKD, whereas DKD has a usual onset time of nearly ten years. Apart from these, lower HbA1c, lower blood pressure, and the presence of hematuria can help distinguish NDKD, though incongruencies between studies have been reported. Notably, microscopic hematuria may be a feature of T2DM patients with biopsy-proven DKD and established proteinuria. Concurrent findings of systemic illness can also help to establish NDKD. IgA nephropathy and prior infection can be strong indicators of NDKD. Hence, it is postulated that renal biopsy can be proposed as a diagnostic tool for NDKD when eGFR is less than 60 ml/min/1.73m2 along with the absence of DR, short duration of diabetes (<5 years), atypical disease progression, presence of hematuria and other systemic diseases as well as nephrotic syndrome.
Unlike DKD, NDKD can be treatable and reversible in many cases. Although DKD is a common cause of CKD, early differentiation can be helpful in isolating treatable forms of NDKD, thereby preventing potential mortality.