Patients with steno-occlusive cerebrovascular disease are at risk of ischemic symptoms from haemodynamic insufficiency in the presence of reversible hypoperfusion, exhausted autoregulation and impaired vasodilatory reserve. Multidisciplinary management approach includes blood pressure management, antithrombotic therapy, treatment of underlying brain-body interactions targeted at optimising cerebral blood flow and oxygen delivery, and revascularisation procedures.
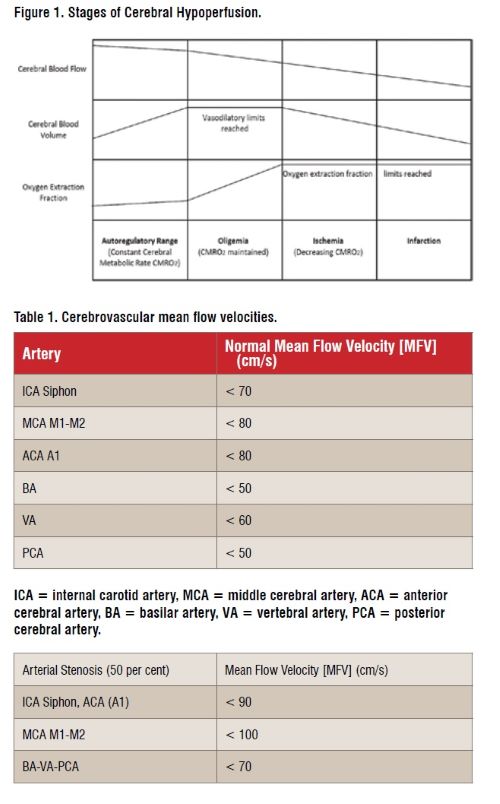
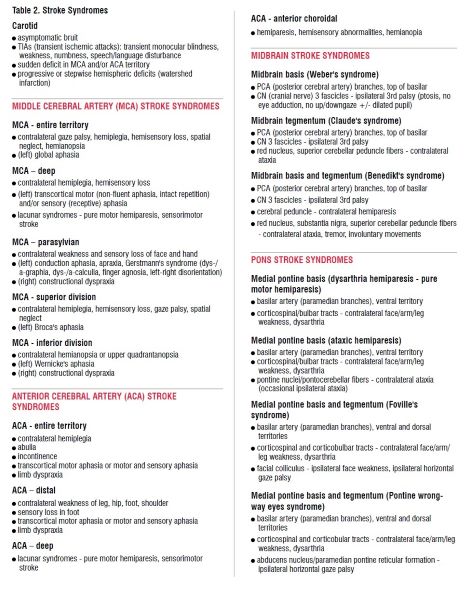
Patients with symptomatic stenoocclusive disease have a risk of recurrent stroke of at least 10-15 per cent within 5 years. Progressive atherosclerosis of internal carotid artery (ICA) or middle cerebral artery (MCA) is the most common cause of impaired distal cerebral perfusion with cerebral misery hypoperfusion (Figure 1, Table 1).

In the setting of cerebral hypoperfusion, recurrent ischaemic events occur depending on the following factors: (1) amount of collateral cerebral circulation; (2) extent of haemodynamic impairment; (3) age; (4) cardiac status; (5) presence of metabolic syndrome of hypertension, hyperlipidemia and insulin resistance; (6) factors affecting coagulation, blood oxygen carrying capacity and delivery (such as anaemia and other haematology disorders, systemic infections and sepsis, renal and hepatic disorders).
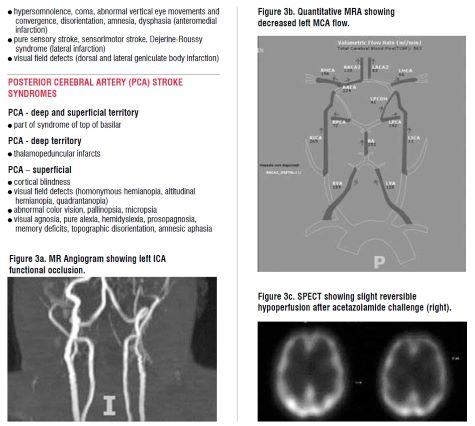
In addition to the traditional cerebral ischaemic symptomatology pertaining to the affected vascular territory (Table 2), orthostatic symptoms, syncope, transient global amnesia, episodic limb shaking and watershed infarction are possible.
In states of misery perfusion, compensatory cerebral vasodilation is not possible as the cerebral autoregulatory capacity is exhausted and, as a result, cerebral blood flow decreases proportionally with cerebral perfusion pressure (Figure 1). Possible cerebral collateral circulation routes include: (1) contralateral internal carotid artery (ICA) through anterior communicating artery; (2) posterior circulation via posterior communicating artery; (3) leptomeningeal or pial collaterals; (4) collateral circulation from external carotid artery (ECA) with retrograde flow and connections with ophthalmic artery, extracranial connections between ECA or vertebral artery (VA) branches and distal ICA; (5) collaterals through dural meningeal arteries to cortical arteries; (6) anterior cerebral artery (ACA)-posterior cerebral artery (PCA) connections via the limbic loop; and (7) anterior spinal artery collaterals with the vertebrobasilar circulation.

Medical management strategies are essential to treatment of cerebral ischaemic events and prevention of recurrent strokes in face of cerebral hypoperfusion. These include: (1) cautious individualised blood pressure management (usually systolic blood pressure targets of 130-160 mmHg for those with severe bilateral carotid stenoses); (2) maintenance of fluid status to maintain appropriate plasma oncotic pressures for adequate cerebral perfusion; (3) anti-platelet and anticoagulant therapies (single anti-platelet agent and anticoagulant for those with embolic strokes or in the setting of cardiac arrthymias; dual anti-platelet therapy, with laboratory evidence of responsiveness to these agents, for those with atherosclerotic disease or perforator events), (4) statin, and (5) glycaemic control.
Treatment of underlying brainbody interactions are also essential, including attention to haemodynamic stability, cardiac status, optimising cerebral oxygen delivery with avoidance of anaemia, goal-directed therapy for sepsis, optimisation of renal perfusion and avoidance of coagulopathy and encephalopathy due to underlying multi-systemic involvement, particularly renal or hepatic impairment.
For patients with symptomatic severe (> 70 per cent) carotid stenosis, carotid endarterectomy or angioplasty/stenting is considered. Thrombectomy is considered for patients with embolic strokes to large size cerebral vessels. For patients who have been medically optimised but are still at risk of ischaemic symptoms of haemodynamic insufficiency due to ICA/MCA stenosis/occlusion in the setting of hypotension or orthostasis, one can identify candidates with reversible hypoperfusion, exhausted autoregulation and impaired vasodilatory reserve. Consideration of extracranialintracranial bypass procedure can be reliably made to identify patients who have reasonable chances of augmentable flow-induced long-term cerebral blood flow re-organisation (collateral shift) while preventing future hypoperfusion events. Identification of these candidates is made after blood pressure management, antithrombotic therapy and treatment of underlying brainbody interactions targeted at optimising cerebral blood flow and oxygen delivery.
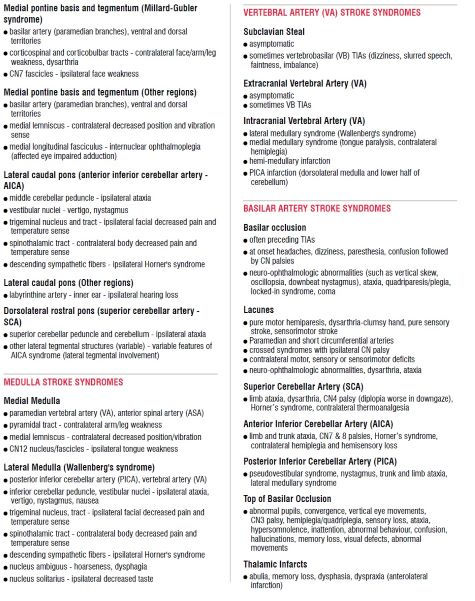
In addition to clinical findings on presentation and with monitoring (Table 2), other adjunctive investigations are useful in identifying such surgical candidates. CT perfusion scans demonstrate ischaemic penumbra of increased time-to-peak (TTP, time between first arrival of CT contrast intracranially and its peak concentration), increased mean transit time (MTT, average time for blood to travel through a volume of brain), with relatively preserved cerebral blood volume (CBV) due to vasodilation and recruitment of collateral flow, and decreased cerebral blood flow (CBF). As reference, an infarcted core shows increased TTP, increased MTT, decreased CBV and decreased CBF. SPECT (single photon emission computerised tomography) scan with acetazolamide (DiamoxTM) is used to identify patients with haemodynamic insufficiency who exhibit reversible hypoperfusion and decreased cerebrovascular reactivity when challenged with acetazolamide (Figure 3a-c). In those who are in the misery perfusion stage of haemodynamic insufficiency, they are already maximally vasodilated and dysautoregulated. In this regard, they cannot further vasodilate in response to increased carbon dioxide tension from diuretic acetazolamide, a carbonic anhydrase inhibitor.
Quantitative MR angiography (q-MRA)’s non-invasive optimal vessel analysis (NOVA) is also essential to quantify and measure blood flow through large vessels of the Circle of Willis (Figure 3b). Together with formal cerebral angiography, it can be used to estimate pial and collateral flow. It gives reasonable estimates of augmentable flow to ensure appropriate blood velocity ranges after bypass, and also in anticipation of longer term collateral shift, cerebral blood flow re-organisation.
Direct superficial temporal artery (STA) [donor] and middle cerebral artery (MCA) M4 cortical branch [recipient] bypass is generally preferred. Meticulous attention to blood pressure control, maintenance of intravascular volume and depth of anaesthesia are essential to avoid cerebral hypoperfusion during these cases with underlying steno-occlusive disease. Intraoperative end-to-side anastomoses are performed using 10-0 nylon sutures with indocyanine green (ICG) and intra-operative angiographic confirmation of anastomotic patency. Individualised blood pressure goals with gradual liberalisation of these parameters are done post-operatively with continuation of antithrombotic agents to maintain anastomotic patency and to avoid reperfusion-related injury.
For patients who have been medically optimised but still at risk of ischemic symptoms of haemodynamic insufficiency due to steno-occlusive cerebrovascular disease, one can identify candidates with reversible hypoperfusion, exhausted autoregulation and impaired vasodilatory reserve. Consideration of extracranial-intracranial bypass procedure can be reliably made to identify patients who have reasonable chances of augmentable flow-induced long-term cerebral flow re-organisation while preventing future hypoperfusion events. Identification of these candidates are made after medical optimisation, including blood pressure management, antithrombotic therapy and treatment of underlying brain-body interactions targeted at optimising cerebral blood flow and oxygen delivery.
Acknowledgement: Acknowledgement is made to Dr. David J. Langer for his expertise in this clinical area.