The patient safety in the operating room commences before the patient enters the operation theatre and includes attention to all applicable types of preventive premedication errors, but surgical errors are unique and need to emphasised. Potentially preventable surgical errors have received increasing attention in recent years. A structured communication pattern between the patient, the surgeon and other members of healthcare team form basis to prevent surgical errors. The surgical environment presents a challenge to safeguard patient safety. These injuries can be serious and advised to monitor patient with the help of checklists, systems, and routines that reduce the chances of wrong-patient, wrong-side, wrong-part surgical errors, and retained foreign objects. Patient safety in surgery demands the complete attention of skilled surgeons using well-functioning equipment under adequate supervision.
Surgical care is a fundamental part of healthcare around the globe. Ensuring surgical safety in operation theatres is the need of the hour. A safe and salubrious operating theatre is achieved only through careful planning, maintenance and periodic checks, as well as proper ongoing training for staff.
An operating theatre is a complex system with numerous risk factors, including not only the features of the structure and its fixtures, but also the management and behaviour of healthcare workers. The Safe Surgery Saves Lives initiative was established by the World Alliance for Patient Safety as part of the World Health Organization’s (WHO) efforts to reduce the number of surgical deaths across the world. Safe surgeries ensure less morbidity and mortality, improved quality of work, less liability, and greater efficiency.

There is increasing evidence that to achieve the full benefit of the checklist, there needs to be an understanding of, and a strategy for, mitigating the technical, socio-political, and psychological barriers to using the checklist. Freestanding surgical units may need to be particularly vigilant in ensuring that personnel and equipment are in good condition for surgery. Protocols and procedures to identify and manage stress and fatigue in surgical personnel may help to avoid surgical errors and patient injuries. The operating room is an appropriate educational environment, but the presence of observers at any level must not be allowed to compromise patient safety. Patient safety in surgery demands skilled individuals using well-functioning equipment under adequate supervision.
Medical errors are inescapable in healthcare profession. The identification of causes and implementation of safety plans to reduce these errors will help to establish an effective patient safety in operation theatres. The causes advocated by WHO are enlisted below:
• Lack of continuous training and education
• Past tolerance of unsafe practice
• Lack of regulations /rules
• Gaps in communication among different healthcare providers
• Gaps in communications between healthcare providers and patients
• Unstable /unreliable systems
• Fear of admission of guilt / wrong doing
• Human factors
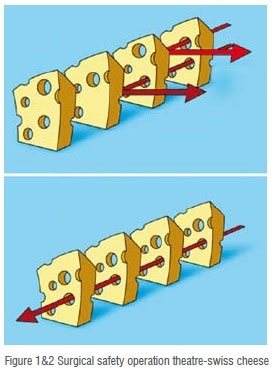
There are various theories which are proposed for system failure. One of the most common is referred to as the “Swiss Cheese Model” of accident causation. Every step in a process has the potential for failure. The ideal system is analogous to a stack of slices of Swiss cheese. Consider the holes to be opportunities for a process to fail, and each of the slices as ‘defensive layers’ in the process. An error may allow a problem to pass through a hole in one layer, but in the next layer the holes are in different places, and the problem should be caught. Each layer acts as a defence against potential error impacting the outcome as described in (Figure 1).
For a an error to happen, the holes need to align for each step in the process allowing all defences to be defeated and resulting in an error (Figure 2). If the layers are set up with all the holes lined up, this is an inherently flawed system that will allow a problem at the beginning to progress all the way through to adversely affect the outcome. Each slice of cheese is an opportunity to stop an error. The more defenses you put up, the better. Also the fewer the holes and the smaller the holes, the more likely you are to catch /stop errors that may occur.
Procedure Scheduling
Scheduling the procedure is very important and is a form of OT planning. All surgery requests should be made in writing and verbal requests by the medical staff should be avoided to prevent any errors in scheduling the procedure. Verification of every document including consent, history, and surgeon orders at the time of scheduling is necessary. Electronic medical records improve the safety process, decreases misunderstandings and missing documents.
Pre-operative measures to prevent errors
A preoperative check up by the concerned doctor gives an added opportunity to correct any mistakes and inconsistencies in the documentation. All discrepancies should be mended at this step before proceeding further with surgical procedure. The informed consent should be duly signed before the procedure. Patient should be explained about the surgical procedure, associated complications, additional procedures, placement of foreign material (Meshes, Plates, Screws, Stents).
The next approach is to mark the site of the procedure to avoid wrong site surgery. The formulated guidelines for marking the site are; involving the patient while performing site marking, to be marked by a licensed practitioner who is responsible for the procedure and the marks should be unambiguous and uniform within the institution and should be semi-permanent to be visible after skin preparation and draping.
The institution should have a written process to ensure that the correct site is operated on. Alternatively, radiopaque markers can be used in the procedures involving fluoroscopy. Surgical armamentarium (e.g. required instruments, guide wires, laser fibres, scopes, stents, loops, prosthesis, etc.) should be verified prior to procedure.
In OT Just Before the Commencement of Surgery
Implementation of safety checklist as proposed by WHO is the main objective at this stage. This helps in improving the outcomes. In a study by Russ S. et al., more than 40 per cent of cases had absent team members, and over 70 per cent of the team members failed to pause and focus on the checks. The timeout is a critical advantage to pause and be sure that the team is aligned about what is being done to whom in which location," Double- and triple-checking a patient's surgical information is worth the extra time to avoid errors. Conduction of timeouts on electronic white boards ensures correct patient identification, site marking, draping and other essential elements are followed. The collaboration of team members in this task is essential at every step for smooth work up.
In the modern age of medicine, digital images, displaying the CT-scan, X-rays on an auxiliary monitor during the procedure act as a guide for surgeons and improve patient safety.
The consequences of positioning related injuries are preventable but can be profound and can result in morbidity, and litigation. Neurological, vascular, musculoskeletal, and pressure ulcers are the most common position related injuries in surgical patients. Neurological complications can be avoided by placing forearms in neutral position or slightly supinated to minimise pressure in the cubital tunnel. It is advised to strap and place them adequately to maintain the correct limb position during the procedure even if the surgical table is moved. The patient’s head should be placed in a neutral position and the arm should not exceed abduction of more than 90° to avoid brachial plexus injury. Straps should not be too tight to prevent ischemia and compartmental syndrome. Padding under osseous prominences can help avoid pressure-related complications. Surgeons must be observant to avoid possible compartment syndrome (limbs) when positioning patients for open, endoscopic, and laparoscopic surgeries.
Collection of Biopsies and Surgical Specimens
A large amount of patients, multiple samples from the same patient, lack of staff, and lack of continuous education and training of healthcare workers account for medical errors. Approximately 1 per cent of general laboratory specimens aremisidentified and can lead to serious harm for patients. Implementation of safety strategies and educating healthcare workers to perform those tasks with as few errors as possible is the mainstay objective. Documentation, writing policies and protocols detailing responsibilities makes the task simpler and avoid errors. To make the process as simple as possible, reducing the number of steps between collecting the samples and receiving the laboratory report should be encouraged.
Procedures that involve biopsy and tissue sampling a specimen may pass through the hands of more than twenty individuals in several workplaces until the final pathology report is given. These handoffs significantly increase the risk of a mix-up and can lead to serious diagnostic errors. Mutual cooperation for supervision of clinicians, technicians, and administrative assistants is essential to prevent and detect errors. The most precarious steps of the biopsy process include labelling of the specimens, appropriate request forms, and accessioning of biopsy specimens. The modern methods for data entry, automated systems for patient identification and specimen labeling, as well as two or more identifiers during sample collection are important steps to reduce misidentification. If misidentification is detected, rejection then recollection is the most suitable approach to manage the specimen. The introduction of innovative methods DNA analysis to assist with correct identification can be used when recollection is not available.

Postoperative Discharge Work up
Planning a discharge has been shown to influence patient outcomes; patient safety can prevent readmissions and improve patient satisfaction. Patient education (Postoperative instruction charts) is when they are discharged home with catheters, stomas, stents, drains, or any other medical device that needs special care. Patient education can reduce complications and improve their quality of life after surgical procedures. Healthcare workers must be aware that language barriers, socioeconomic status, and age can impact patient comprehension of instructions.
Medication Safety During Administration
Medication safety is ensured by applying the five R’s: right drug, right route, right time, right dose, and right patient. Medication errors are barriers that prevent the right patient from receiving the right drug in the right dose at the right time through the right route of administration at any stage during medication use, with or without the occurrence of adverse drug events.
Modern systems of information technology, such as computerised order entry, automated dispensing, barcode medication administration, electronic medication reconciliation, and personal health records are essential in the prevention of medication errors. Electronic medical records help in rapidly screening the medication regimens of hospitalised patients and deliver timely, point-of-care intervention when indicated.
The most common prescribing errors are incorrect drug, incorrect dose, allergies, and drug-drug interaction. It is important to tailor prescriptions for individual patients, identifying allergies, pregnancy, lactation, age, co-morbidities. Healthcare workers must be familiar with the medications they prescribe and need to know the medications in their specialty that are associated with high risk of detrimental effects. Drug interactions can lead to serious adverse events or decrease drug efficacy. Prescribing health-care workers should ask patients of any use of over-the-counter medications or dietary supplements because they are frequently under reported and may cause drug interactions. Prescribing the generic name of drugs simplifies the communication among healthcare workers, reducing errors. However, patients need to be educated that their medication may be called by different names (brand and generic name) and they should be encouraged to keep a list of their medications, including both the brand and generic name of each drug.
Education and Training of Healthcare Workers
Formal training to doctors, nurses, and other operating room staff is essential to help foster a team approach. This helps in break-down of the hierarchy present in the operating room. The nurses and other operating room staff should be more comfortable in questioning the physician if they felt that something was going wrong. This operational behaviour forms a pillar of strength in operation theatres.
Technological advances, novel surgical devices, and minimally invasive techniques are rapidly increasing within the surgical community. Concerns about device safety and training are increasing, making it important to protect patients from harm. Devices need to be extensively evaluated in research before and after FDA approval.
The residents are subjected to follow a pre-planned schedule during their duty hours and it is imperative to consider ensuring that patient safety is not jeopardised by breach in the care. The handover process is the bridge to continuity and safer patient care. Medical educators and clinicians should work toward adopting and testing principles of optimal handover processes in their local practices by applying the knowledge of patient safety issues discussed in this report.
Conclusion
It is better to be safe than sorry. The universal operative procedure for OT etiquette is to be followed to decrease the risk of random inappropriate practices. The voluntary pre-operative briefings in the operation theatre allows the surgeon to make the process on their own. The overall acceptance is slow and adherence to the protocols in operation theatres will be more robust if every surgeon claims ownership. A good and well furbished OT set up with implementation of staff education will prepare the healthcare personnel to reduce the probability of unwanted incidents—delivering safe, effective, and a high standard of care to all patients.
Acknowledgment
I thank Dr. Rajesh Sardana, medical writer, Max Institute of Minimal Access Metabolic and Bariatric Surgery for compiling the content of article.