Health Equity is not only poorly understood but poorly managed in most organisations and countries. The difference between equity and equality needs to clear. The leaders path to address these basic issues for Staff, those we serve, and the community is not complex, it is just very hard.
Health equity is a hot topic. It is a common issue rolled out by leaders when describing their vision for their high-performing healthcare institutions. It receives thoughtful nods, clear verbal support and declarations of it being a priority. But if they are pressed to describe specific progress they are making…or even what exactly they include in their definition of Health Equity, things get less firm very fast. Many will point out they have a policy in HR that addresses equity, or that they have a code of conduct among their staff that insures they would always treat everyone ‘equally’. Some have even received national awards and have been recognised by their community as a great partner on many important social projects. Surely that all adds up to delivering on health equity?

But this is exactly the problem. Because many organisations have done those things, we assume we must be making significant progress. It is true those things are necessary, but they are woefully insufficient.
Derek Feeley president of the largest international healthcare improvement organisation, Institute for Healthcare Improvement1, says Health Equity is one of the least well understood and most difficult to demonstrate significant progress of the Six Pillars put forth by the IOM2:
• Safe: Avoiding harm to patients from the care that is intended to help them
• Effective: Providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding under use and misuse, respectively)
• Patient-centred: Providing care that is respectful of and responsive to indi-vidual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions
• Timely: Reducing waits and some-times harmful delays for both those who receive and those who give care.
• Efficient: Avoiding waste, including waste of equipment, supplies, ideas, and energy
• Equitable: Providing care that does not vary in quality because of personal characteristics such as gender, ethnic-ity, geographic location, and socioeco-nomic status.
The most universally used definition for health equity comes from The World Health Organisation3:
“The absence of avoidable or remediable differences among groups of people, whether those groups are defined socially, economically, demo-graphically, or geographically. Health inequities therefore involve more than inequality with respect to health deter-minants, access to the resources needed to improve and maintain health or health outcomes.”
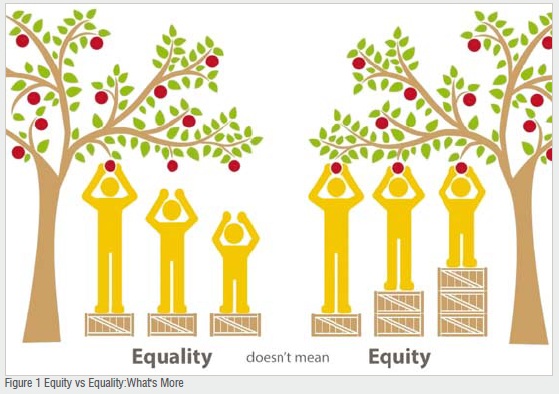
A very import feature is that it draws a clear distinction between equity and equality. Being clear in your language that you have equal access for employ-ment, equal access to care or equal opportunities in your community for people to partner barely scratch the surface of heading in the direction towards equity. Equality always favours the better educated, better resourced, better connected. Equity addresses issues based on the situation of those served. The figure below helps solidify this concept.

Next we need to appreciate the breadth of the issue. Alan Weil in Health Affairs4 gives us strong examples of the scope of how the problem is far beyond the very important and unsolved issues of race and gender. Inequity is also prev-alent with struggles related to age, sexual orientation, socioeconomic status, food water and power availability to name several of the top few. With this large group of issues staring us in the face, there is no chance an HR policy, no matter how thoughtful will serve this need. It will take broader thinking, courage to take a stand and discipline to follow through. Beyond the huge moral imperative there is a significant strate-gic advantage to take on these difficult changes in how we function. Health Equity must be a Strategic Priority5
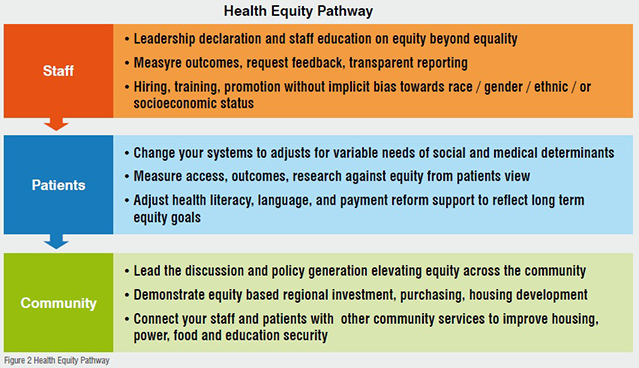
A clear path forward as a leader of the healthcare organisation is not to get buried by the expanse of this responsibil-ity but to break into manageable pieces that you can make measurable progress on in a definable future timeline. Your role is to set Equity as a priority and then teach how progress can be made in the three major areas of opportunity, see figure 2:
As you can see the major efforts would be attention to your own staff, the activity of your staff in relation to your patients, and then finally your connection with your community.
You’re not alone in any of these. The diagram shows there are multiple opportunities to interact with people that have started this work to help guide your efforts and make you more efficient and more effective. It will improve your organisation will prove your community and will give you both a mission consist-ent and a competitive way forward.
The plan is not complex, it is just hard. First, you need to call equity out as an issue that is going to be a part of the core functioning of your organisa-tion. Verbally, in writing, and in the consistent deeds of the senior leaders there can be no doubt on what accept-able behaviour is going to look like and act like in regards to race, gender, age or the many other issues where equity can be a problem. This cannot be left in HR policy. It needs to be clear to all leaders regardless where they are in the hierarchy that this is the only path forward…not optional…not intermittent. This is an important and measurable part of every-one’s work. A recent article in the Asian Hospital & Healthcare Management6 has several easy to use tools to get started with then modify to fit your needs. You can’t possibly expect your staff to treat your patients in an equitable manner if your staff is not treated similarly. - M. Bisognano (Thompson, page 92).
The treatment of your patients can no more be left to chance than the treat-ment of your staff. It has to be clear and explicit the patient will be given equitable (not just equal but equitable) care delivery in all settings at all times. If someone feels that is not possible, a system needs to be in place to raise the issue up to the level of senior leader-ship. Outcomes need to be searched for on both staff and patient evaluations. Without asking the impact of frontline decisions may not be perceived by even diligent senior leaders.
One might say those two pieces of work (staff and patients) are enough for the next decade. It certainly is a large task and very few of organisations have really accomplished anywhere near what needs to be in those two areas, but the third is equally important.
If healthcare is going to move out of the business of sitting in our boxes wait-ing for sick people to show up and move into the communities and show that we are a true partner to improve broad health and well-being, then we have to do that in a way that is grounded in equity. It is a very short walk in most communities to go from the healthcare institutions to neighbourhoods with limited resources for the basics of food, housing, or power. Although you might argue that those are all responsibilities of the government or individuals, the best science shows that we will make little gain in the health of the community without addressing these as well as “sick” care problems. BMC Medicine7
You do not have to figure this path way on your own. There are many resources to help. For example the group called Health Leads8 has developed a roadmap to help address social determinants like housing, food, and power. Their advice could be found at Health Leads and can be modified for multiple diverse settings. It can be started with very small time and materials but get you on a path to have these critical conversations, build a plan, and start moving forward. Asian Food Security9.
If we are going to be a partner and leader and be seen as a major asset rather than just a business, then we need to look to the availability and distribution of food and housing. We need to use our economic power to source local materials, to hire in an equitable fashion, to share our inclusive staff development programs, to build connections with the schools to help prepare all for their future opportunities not just those who are already doing well. We have the ability to influence local and regional investment by how we behave and how we use our assets. It has been shown in multiple situations the positive influence on the growth and development of communities if healthcare truly lives its mission of improving the health and well being of the whole community. Not just the easiest or those who already have the most assets.
Another resource, The Health Anchor Network10 has published several documents to help you get started inequitable hiring, training and investing in local communities. There are examples of great successes of small startup investments or tens of millions dollars. These examples are not limited to North America. Across Asia there are many organisations that are pushing forward leadership training (Equity Initiative11) as well as large gatherings of like-minded leaders, for example - International Forum on Quality and Safety in Healthcare: Asia-Pacific12. The focus is on getting started to not just do something but accomplishing something in an equitable manner to serve the mission and our communities. Health Equity must be a Strategic Priority13 / Building a Culture of Health14.
In summary, we have to move past the illusion that an HR policy or a directive to the staff is somehow accomplishing health equity. It will take a concerted effort with our own employees to be clear about the expectations, a system to help them stay on the path and consistent leadership to help move this to our patients and families. The community will need this same leadership to help set a course that is both morally sound but strategically advantageous. Raising everyone up will strengthen the fabric of the community.
It is unlikely to have economic health with out personal health. And it is unlikely to have personal health within a weak economic environment. They complement each other. We are better off if all can come along in both of these dimensions. This is a great opportunity to lead forward on equity. This is a very difficult problem that no one has really solved. It gives you a chance to show that you can start making measurable progress and live up to the values, mission and vision of your organisations.
References:
1. http://www.ihi.org/Pages/default.aspx
2. https://www.ahrq.gov/professionals/quality-patient-safety/talkingquality/create/sixdomains.html
3. http://www.who.int/healthsystems/topics/equity/en/
4. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.0583
5. https://catalyst.nejm.org/health-equity-must-be-strategicpriority/
6. https://www.asianhhm.com/healthcare-management/becoming-world-class-with-class
7. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-015-0342-3
8. https://healthleadsusa.org/tools-item/the-social-needsroadmap/
9. https://www.ncbi.nlm.nih.gov/pubmed/19965356
10. https://www.healthcareanchor.network/
11. http://www.equityinitiative.org/who-we-are/
12. http://internationalforum.bmj.com/melbourne/
13. https://catalyst.nejm.org/health-equity-must-be-strategicpriority/
14. https://www.rwjf.org/en/how-we-work/building-a-culture-of-health.html