Emergency Departments (ED) usually function with limited staff trained for its proper functioning. During times of surge, the situation gets complicated due to non-availability of sufficient resources. Telehealth technology, through its ability to bridge the physical divide between casualties and their care providers, is could to be very successful in helping to deliver higher levels of care. This article discusses how this is made possible.
Emergency departments by nature exist to take care of those that are critically ill and demand attention of an immediate nature to lessen mortality. They require personnel with special skills to be able to discharge their required functions most effectively. For a number of reasons, such personnel are not available in sufficient numbers at the best of times. Their paucity is particularly felt during times of surge when all the available resources in terms of personnel and material are employed to over-capacity and fresh arrivals threaten to throw the entire effort off-gear more frequently than what is comfortable.
Many times it makes more sense to treat those in need of attention in the field or at locations that are not geared up for emergency medical care in terms of the right personnel even if much of required equipment may be available. In such instances, telehealth technology can act as a “care multiplier” of sorts by having the specialists be available virtually instead of physically. This helps in enabling the delivery of better care leading to better outcomes in terms of both morbidity and mortality.Let’s look at the ways and means of how this can be accomplished.

Telehealth technology can be defined as the employment of modern day telecommunications and information technology to help provide healthcare services anytime anywhere. Mobile technology, hand-held devices, the cloud, smartphones, tablets, ability to handle big data, Hadoop systems, Map Reduce, connectivity using Wi-Fi, Bluetooth®, Near Field Communication (NFC), QR codes, authentication using One Time Passcode (OTP), message encryption-decryption technology, etc., are all helping make telehealth emerge from the pages of articles and the ivory towers of academia to help transformation of healthcare delivery a reality.
On any given day, the emergency department is typically a beehive of activity. At out-of-office hours (read outside-of-OPD timings) it is usually the first port of call for any person with a health issue. Unfortunately world-wide, the department is almost invariably short of well-trained staff due to a variety of reasons, one of which is high rates of burnout due to high stress. Emergency care is the doorstep of critical care, where time is of the essence. Clinical situations handled within the “golden period” proves crucial to a successful outcome more often than not.
During epidemics or situations with mass casualties, the emergency department, and consequently emergency care, resemble more of a fall-out shelter and often an extension of the disaster zone if the facilities are located in proximity. In fact, it is nothing short of a picture of utter chaos during times of surge with patients dead or dying being placed in any are that happens to free at that time and providers having to mill about in any available free space, often leaping over people and equipment, many of whom are not normally accustomed to dealing with anything like it.
This leads to a situation where a department already working at maximal or even beyond maximal capacity is forced to deal with an overwhelming situation. Although with an “all hands on deck” approach by all available personnel this situation is handled, the paucity of the “right” kind of personnel capable of making the difference forces the situation to be somewhat hamstrung from the very beginning. At this point, any help of any sort is more than welcome. Unfortunately, it is the human resource, so vital to make a difference between living and dying, that is in severely short-supply.
The situation, therefore, is clearly helped by something that would alleviate, even partially, the lack of availability of the experts. This is where telehealth technology can come to the rescue in a very significant manner. Through its ability to successfully “bridge” the physical distance between the care provider and receiver, it permits experts to provide care to people who need it irrespective of where they are actually located.
However, telehealth is not just limited to “bridging the physical divide” through a variation that can loosely be termed as tele-consultation. It is capable of doing a whole lot more. To name a few, it can help the outputs of monitors and other assisted living devices including ventilators and pressure sensors to adjust body positions to be telemetered through to the remote experts coupled with the use of appropriate rules-based alerts and triggers that prioritise provider focus and auto-initiate actions to help in providing optimal care.
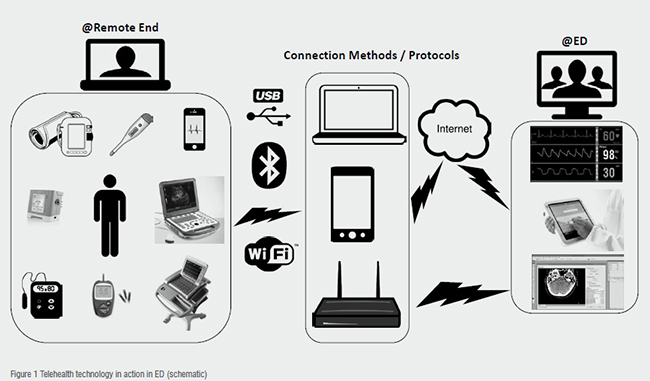
A schematic diagram accompanied by a brief explanation is provided below to help illustrate this concept and understand the methodology that can be used to augment care in times of surge in the emergency department.
Telecommunications technology in terms of communication protocols are used to connect various monitors and audio-video equipment via the Internet and or direct networking to the emergency department. Information technology is used to process the clinical data collected at remote locations and present to the emergency and critical care specialists located in the ED for necessary action.
The specialists can then take an appropriate decision to either evacuate a casualty to the emergency department or treat the person locally, based on their informed clinical assessment regarding the most likely outcome, level of ability to be brought across, degree of injury, etc. The triage may even reveal that the likelihood of an optimal outcome is more if treated at the remote location than being brought across to the ED by providing guidance from a distance to less experienced and/or less qualified personnel.
Telehealth technology has the potential to, and indeed can, deliver the much required care multiplier capabilities to all areas of healthcare. The visible impact of which would be most apparent in the areas of critical care and emergency services, that is precisely those areas that need high levels of skills and expertise to help ensure lowering of mortality in highly morbid cases. Sadly, the technology is ill-understood, as a consequence of which it remains abominably under-utilised. The sooner the stakeholders such as providers, authorities, payers, and particularly the patient, begin to appreciate the immense potential it holds, the sooner will it be appropriately harnessed to help keep people healthy and attain the goal of WHO of health for all aka universal healthcare.
References: A DIY Guide to Telemedicine for Clinicians, Dr SB Bhattacharyya, Springer 2017, ISBN 978-981-10-5304-7