Effort to develop successful mechanical circulatory support started at the same time with the development of cardiopulmonary bypass for safe open heart surgery in 1950s. After the beginning of heart transplantation, necessity of mechanical circulatory support (MCS) become evident because patient need a bridge time support up to the availability of donor organ. Contraindications to heart transplantation and lack of donor heart further stimulated the development of long term mechanical circulatory support. But it is very important to select the device for a particular patient, whether need a temporary device or permanent.
Advanced heart failure patients are severely ill and have exertional dyspnea on minimal effort or even at rest. Hemodynamic instability is so severe that need multiple inotropic support, mechanical circulatory support or even heart transplantation.
Most of these patients are in the hospital on support. Many of the patients have to wait for a long times for heart transplantation. Patients who are ineligible for heart transplantation due to underlying medical conditions may take the service of MCS for the beneficial effects of it.
Decades of research has enabled durable mechanical circulatory support devices that are widely available now. The recent advancement in pump technology produced the left ventricular assist system and reduces the burden of advanced heart failure management.
Candidate selection for MCS service, risk stratification, and management strategies change with the development of new pump technology. As do profiles of patients according to MCS device.
After the first human heart transplant by Cristiaan Barnard in December 3, 1967, artificial ventricle technology began to be used as a mechanical bridge to support patients with post-cardiotomy shock until a donor organ could be available. In 1969, Cooley et al., reported the first use of a total artificial heart as a bridge to transplant (BTT).
In the early 1970s, heart transplantation faced a difficult period of high mortality due to transplant rejection due to inadequate immunosuppression. That accelerated the development of MCS.
However, the first generation LVADs of the 1970s could only support for a matter of days. For these limitations the NIH authority of USA had to issue another series of initiatives in the late 1970s to develop durable implantable assist devices intended for use in chronic heart failure (Figure 1).
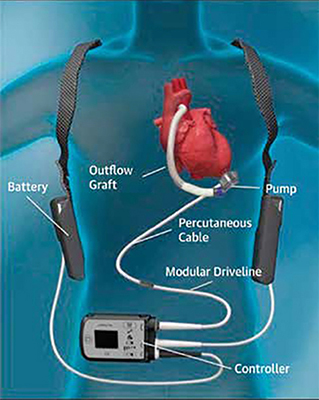
Figure 1: Left ventricular assist device (LVAD)
The interest of mechanical circulatory assist technology came in 1982 after Barney Clark, a Seattle dentist, received the Jarvik-7 total artificial heart (TAH). But TAH development almost stopped because of high rates of infection, pump thrombosis, and stroke.
At the same time, cardiac transplantation experienced a renaissance after the US FDA approved cyclosporine in 1983. Improved immunosuppression featuring a calcineurin inhibitor contributed to a sharp increase in graft survival and a rapid expansion in the number of heart transplant programs in the United States.
Continuous flow pumps started replacing previous pulsatile technology in 2008 and covered completely by 2010 due to more complication rate. With this shift of pulsatile to continuous flow pump, another development occurred at the same time and that is small pump profile to allow easy intrapericardial implantation.
Device durability increased with continuous flow left ventricular assist device (LVADs) but risks of bleeding, stroke, infection remains together with device malfunction or failure.
For patients with irreversible biventricular failure TAH can help in this regard. But same type of problems of LVADs accompany the TAH technology (Figure 2).
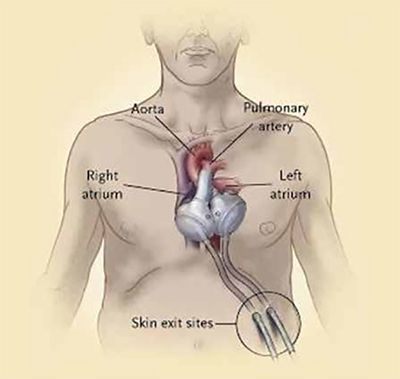
Figure 2: Total Artificial Heart (TAH)
Another important trend in pump development has been miniaturization, even at the expense of flow rate. HeartMate III heart pump (weight 200g, measuring 50.3mm in diameter and 55.8mm in height, including inflow cannula) has bearing less motor using magnetic levitation (Full MagLevTM Flow Technology), able to fit intrapericardially and has less chance of pump failure.
Smaller pump design can be used in both acute insult or cardiogenic shock and chronic heart failure. So, it can help the heart to recover ventricular function in case of acute insult and to provide durable assistance in chronic failure.
Every therapy designed to increase survival must be judged in part not only by those events or complications that diminish survival but also by those that help define the quality of life anticipated. For device therapy, the critical adverse events include device malfunction or failure, neurologic events, and infections. From the early analyses, about 10 per cent of patients developed significant device malfunction within the first six months. Cardiovascular failure, central nervous system events, infection, liver failure, and respiratory failure were the most frequent causes of death. It is hoped that the precision and consensus underlying this effort will level the playing field and accelerate the reduction of complications for current and future device development.
In case of advanced heart failure patient, it is observed that few pathology of the patient are predictors of high mortality even if we use more than one modality of treatment. As for example, pulmonary hypertension increases risk of mortality in medical therapy and also in heart transplantation. In patient with right ventricular failure, mortality increases with medical therapy and mechanical ventricular assist. If advanced heart failure patient has renal dysfunction, there is chance of more complication during management and also more mortality even with all modality of medical and surgical approach.
Actually current and future research should focus to fix the clinical indicators of advanced heart failure patient that can predict the poor survival with standard heart failure therapies. So, ventricular assist technology can be considered in appropriate time and patient can get maximum benefit from this treatment modality.
In Bangladesh, circulatory support devices have little application. National Institute of Cardio-Vascular Diseases (NICVD) had a Datascope IABP machine since the 1990s. This device was first used in 1997. Off Pump CABG was demonstrated in Bangladesh for the first time by a French surgeon Dr Akter Ali Rama at that time. One of the patient developed low output syndrome and he used IABP then. Now IABP is available in all cardiac centres. The first use of ECMO in Bangladesh was in 2013. Now it is available only in four centres (three in Dhaka and one in Sylhet district). A CentriMag device also ready for use in a hospital of Dhaka. The first implantation of durable LVAD in Bangladesh happened recently in United Hospital Dhaka on the 2nd of March 2022. A HeartMate III device was successfully implanted in a 42-yearold patient.
In recent years, the rapid progress of MCS technology has increased survival and improved quality of life for selective patients with advanced heart failure. And there is a meaningful option generated for lifelong support even in patients who are not candidates for transplantation. With these advances have come new challenges and opportunities.
References:
1. Anisuzzaman DM. Heart Surgery: Past, Present and Future. LAP LAMBERT Academic Publishing, Chisinau, Moldova, 2021. ISBN: 978-620-3-92456-5.
2. Stewart GC, Givertz MM. Mechanical Circulatory Support for Advanced Heart Failure; Patient and Technology in Evolution. Circulation. 2012;125:1304-1315.
3. Cooley DA, Liotta D, Hallman GL, Bloodwell RD, Leachman RD, Milam JD. Orthotopic cardiac prosthesis for two-staged cardiac replacement. Am J Cardiol. 1969;24:723-730.
4. Netuka I, Schmitto JD. Fully magnetically levitated left ventricular assist system for treating advanced heart failure: A multicenter study. J Am CollCardiol.2015;66(23):2590-2593.
5. DeVries WC, Anderson JL, Joyce LD, Anderson FL, Hammond EH, Jarvik RK, Kolff WJ. Clinical use of the total artificial heart. New Engl J Med. 1984;310:273-278.
6. Hunt SA, Haddad F. The changing face of heart transplantation. J Am CollCardiol. 2008;52:587-598.
7. Strueber M, O’Driscoll G, Jansz P, Khaghani A, Levy WC, Wieselthaler GM. Multicenter evaluation of an intrapericardial left ventricular assist system. J Am CollCardiol.2011;57:1375-1382.
8. Copeland JG, Smith RG, Arabia FA, Nolan PE. Cardiac replacement with a total artificial heart as a bridge to transplantation. N Engl J Med. 2004;351:859-867.
9. Kirklin JK, Naftel DC. Mechanical Circulatory Support: Registering a Therapy in Evolution. Circ Heart Fail. 2008;1(3):200-205.
10. Anisuzzaman M, Hosain N, Rahman MR. Mechanical Circulatory Support: Historical Perspective. Cardiovasc J. 2022;15(1):75-80.