The number of adults with congenital heart disease (ACHD) is increasing and heart failure (HF) is often the reason of morbidity and mortality. Heart transplantation is still the gold standard to treat advanced HF and here an international network is needed to collect data on ACHD listed for the heart- or heart and combined organ transplantation to elucidate treatment in this patient cohort.

During the past decades and due to the improvements in cardiology and cardiac surgery, the number of adults with congenital heart disease (ACHD) has increased and so has the need to treat the consequences of palliative or corrective surgery in the youth. In fact, the number of patients with ACHD has increased by about 50 per cent compared with the number of children with congenital heart defects since the beginning of the new millennium, and prevalence of complex lesions is increasing due to a better survival in patients with moderate or complex congenital heart disease. Although ACHD may present with conditions related to general cardiovascular risk factors like coronary artery disease, by far the most common diseases leading to morbidity and mortality encountered by physicians are arrhythmia, heart failure and thromboembolic events. For arrhythmia management, current recommendations regarding ablation and device therapy have to be considered including special anatomical considerations as well. Further, there are implications regarding heart failure treatment in the background of the different anatomical conditions with involvement of the anatomic left or right ventricle as systemic ventricle or with single ventricle physiology.
ACHD with a complex anatomy have a high likelihood of developing heart failure which is related to the underlying congenital heart defect. In this context HF has been reported in 22 per cent of adults with transposition of the great arteries and following atrial switch surgery (Senning or Mustard operation), 32 per cent of ACHD with congenitally corrected transposition of the great arteries, and 40 per cent of ACHD with univentricular circulation and most commonly Fontan surgery previously. Before this background, it is important to point out that HF is responsible for approximately 20 per cent of mortality during early adulthood in ACHD and the current guidelines for therapy of HF cannot be directly applied to these patients as ACHD is often excluded from heart failure trials.
The reason ACHD represents a unique population of patients being prone to develop HF is elucidated with some of the aspects which have to be considered in this cohort of patients.
a.Morphology of the systemic ventricle: In some of the ACHD with complex anatomy like transposition of the great arteries and atrial switch operation, hypoplastic left heart syndrome following palliative surgery or congenital corrected transposition of the great arteries the anatomic right ventricle is the systemic ventricle and responsible for the systemic circulation instead of the low pressure lung circulation. Due to a different structure of the muscle layers of the right ventricle, with only two muscle layers, instead of three muscle layers as in the anatomic left ventricle. The anatomic right ventricle is unable to sustain the pressure generation for the duration of a normal patient’s life and is prone to develop heart failure which is difficult to treat due to the lack of evidence-based treatment recommendations regarding medical therapy.
b. Pulmonary arterial hypertension: The development or presence of pulmonary arterial hypertension is a common comorbidity as a result of different underlying types of congenital heart disease. Most often these patients have a diagnosis of shunt of the circulation on the atrial, ventricular or arterial level. Thus, careful evaluation of haemodynamic data, clinical presentation, and laboratory results are needed to evaluate if pulmonary arterial hypertension is complicating the disease in ACHD. In ACHD the disease type is most commonly type 1 according to the World Health Organization (WHO) classification and pulmonary vascular resistance is elevated with ≥3 Wood units. In this context, it is important to point out that some of the patients as well might have an increased pulmonary wedge pressure when the systemic ventricle has an impaired function often present in transposition of the great arteries following atrial switch operation or in patients with congenital corrected transposition of the great arteries.
c. Shunts, collateral arteries, buffles following surgery: In patients with complex underlying congenital heart defects, shunts or collaterals of arteries are often present being a residual state following initial corrective or palliative surgery. In this context, localisation of the shunt is of importance as the location of a pre-tricuspid shunt, like in the case of an atrial septal defect, will result in a volume load of the pulmonary circulation whilst post-tricuspid shunt lesions with the most common being a ventricular septal defect, cause volume load of the left ventricle. Baffles the following surgery may be prone to narrow with passing time and might be causing exercise limitation due to limitation of the filling of the ventricle.
d.Arrhythmias: The prevalence of arrhythmias is increasing as patients; these arrhythmias might be a consequence of altered anatomy, including the heart conduction tissue, and as well a result of residual or postoperative sequelae. In ACHD the whole spectrum of arrhythmias can be encountered and often several types coexist including disorders of the sinus node, AV-node, His-Purkinje system or intra-atrial propagation. In several types of congenital heart disease, ventricular arrhythmias are the leading cause of sudden cardiac arrest and thus mortality with a 100-fold increased risk in comparison to an age-matched control population. However, the incidence for this often fatal event is only 0.1 per cent and the highest risk is present in patients with Tetralogy of Fallot, univentricular hearts, or patients after Senning or Mustard procedure and transposition of the great arteries. As a consequence, the treatment of ACHD with device therapy including pacemakers or defibrillators is based on few studies although the treatment with devices is an important aspect in HF patients with potential fatal arrhythmias or cardiac resynchronisation therapy, which is often established in HF patients with reduced ejection fraction and left bundle branch block.
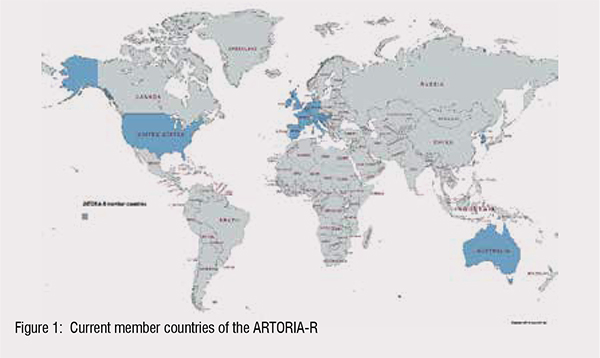
The pAtientspResenTing with cOngenitalheaRtdIseAseRegister (ARTORIA-R) is an international, observational project collecting retrospective data from 16 countries in the time period 1989 to 2022 and will thereafter include data prospectively (Figure 1)1.
This recently started registry will include data regarding the anatomy of the underlying congenital heart disease, pre- and post-transplant status of the patient, and waiting list details. Study partners are welcome to share their data with the registry and in return are allowed to use the data for scientific projects.
The study is registered at ClinicalTrial.gov (https://www.clinicaltrials.gov/) of the United States Library of Medicine with the identifier: NCT04848844
The listed aspects are a selection of the most important reasons why ACHD treatment has to be considered differently as well as decision making regarding advanced heart failure therapies.
Due to the increasing number of ACHD incidences worldwide and an increase of subjects with the development of heart failure, treatment considerations have to be adapted to this population of patients. Thus, an issue for these patients is that randomised treatment studies are often lacking or are futile to start due to the low number of patients in the context of the overall patient number with heart failure. An option to generate and collect more data in this patient population is analysing data of registry information of ACHD listed for heart or heart and combined organ transplantation and thus a cohort with advanced heart failure.
The study has been reviewed, in individual countries, in line with national requirements for ethical approval and followed according to local protocols for data management.
a. they are listed as an adult transplant candidate (≥18 years) for heartonly or heart-combined with other organs.
b. they have a congenital heart defect
c. data is available from the initial evaluation for listing or the first listing on the waiting list.
d. data of patients with advanced HF evaluated for listing but being in a too poor condition to be listed are entered as well.
e. transferred data is anonymised.
f. The institution/organisation agrees to the data management and scientific cooperation plan.
if they are listed for a second heart transplantation (retransplantation).
The suggested register will contribute to the scientific progress regarding treatment of advanced HF in ACHD and in this aspect as well contribute to the improvement of clinical care of ACHD in Europe but as well in the international scope. Thus, with a large cohort of subjects reflecting the current standard of treatment and care of HF in ACHD, implications regarding a certain treatment or intervention can be made which might lead to a consensus regarding future treatment of this patient cohort.
In summary, in the background of increasing numbers of ACHD and thus a challenge to treat heart failure in these often young patients more international networking is needed to address this still unmet worldwide heart care problem.
References:
1. Sinning C, Zengin E, Diller GP, Onorati F, Castel MA, Petit T, Chen YS, Lo Rito M, Chiarello C, Guillemain R, Coniat KN, Magnussen C, Knappe D, Becher PM, Schrage B, Smits JM, Metzner A, Knosalla C, Schoenrath F, Miera O, Cho MY, Bernhardt A, Weimann J, Gossling A, Terzi A, Amodeo A, Alfieri S, Angeli E, Ragni L, Napoleone CP, Gerosa G, Pradegan N, Rodrigus I, Dumfarth J, de Pauw M, Francois K, Van Caenegem O, Ancion A, Van Cleemput J, Milicic D, Moza A, Schenker P, Thul J, Steinmetz M, Warnecke G, Ius F, Freyt S, Avsar M, Sandhaus T, Haneya A, Eifert S, Saeed D, Borger M, Welp H, Ablonczy L, Schmack B, Ruhparwar A, Naito S, Hua X, Fluschnik N, Nies M, Keil L, Senftinger J, Ismaili D, Kany S, Csengeri D, Cardillo M, Oliveti A, Faggian G, Dorent R, Jasseron C, Blanco AP, Marquez JMS, Lopez-Vilella R, Garcia-Alvarez A, Lopez MLP, Rocafort AG, Fernandez OG, Prieto-Arevalo R, Zatarain-Nicolas E, Blanchart K, Boignard A, Battistella P, Guendouz S, Houyel L, Para M, Flecher E, Gay A, Epailly E, Dambrin C, Lam K, Ka-Lai CH, Cho YH, Choi JO, Kim JJ, Coats L, Crossland DS, Mumford L, Hakmi S, Sivathasan C, Fabritz L, Schubert S, Gummert J, Hubler M, Jacksch P, Zuckermann A, Laufer G, Baumgartner H, Giamberti A, Reichenspurner H, Kirchhof P. Study design and rationale of the pAtients pResenTing with cOngenital heaRt dIseAse Register (ARTORIA-R). ESC Heart Fail. 2021 Dec;8(6):5542-5550. doi: 10.1002/ehf2.13574.