Misunderstanding of the natural history of the disease, lack of screening programmes, and reliance on the degree of stenosis as the sole determinant of intervention are important factors contributing to a wide gap in the management of aortic stenosis. We present tools to narrow this gap through series of studies conducted on a large cohort of patients.
Aortic stenosis (AS) is the most common valvular heart disease in Western countries and is expected to become a larger healthcare concern as populations continue to age and the burden of atherosclerotic risk factors concurrently increases. Prevalence of moderate or severe AS in patients 75 or older is 2.8 per cent, and the number of patients with AS in the United States is projected to more than double by 2050. AS carries a high risk of morbidity and mortality even in early stages of the disease, and the only available treatment is aortic valve replacement (AVR).
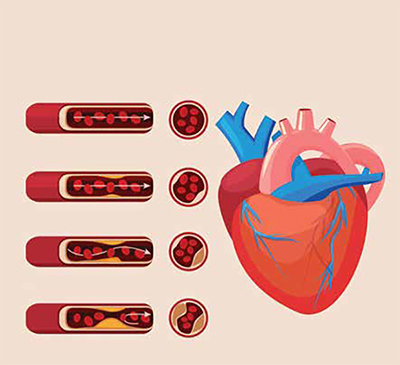
AS initially develops by endothelial injury and dysfunction, inflammation, progressive remodelling, and calcification. This process stiffens or fuses the valve leaflets, which inhibits their separation during systole. The stenosis impedes left ventricular ejection and increases left ventricular systolic pressure, resulting in compensatory adaptive changes such as concentric hypertrophy. Initially, ejection fraction, cardiac output, and left ventricular end-diastolic volume are maintained, and patients may have a prolonged asymptomatic period. However, as the degree of stenosis and hypertrophy worsens, AS becomes clinically significant. Common symptoms include dyspnea, decreased exercise tolerance, dizziness or syncope, and angina pectoris.
AS can be stratified into mild, moderate, and severe through haemodynamic staging. Although patients with moderate and severe AS experience high morbidity and mortality, AVR is typically reserved for patients with severe AS, when the risk of death of AS outweighs the risk of surgical mortality. The current definition of severe AS is based on studies showing that a maximum flow (Vmax) > 4 m/s aligns with the onset of symptoms in 70-80 per cent of patients. While onset of symptoms marks a significant increase in mortality, up to 50 per cent of patients with AS are asymptomatic and still have high mortality. Because AVR has been shown to increase longevity and improve quality of life, studying patient risk factors in conjunction with echocardiographic findings can help inform decisions on the timing of intervention.
In our experience, we found that all degrees of AS are associated with higher mortality risk compared to subjects with no AS. We studied 37,131 patients over six years period. These patients were then stratified into five groups (A-E) according to Vmax percentile (Group A: Vmax<75th percentile, Group B: Vmax between 75th and 90th percentile, Group C: Vmax between 90th and 97.5th percentile, Group D: Vmax between 97.5th and 99th percentile, Group E: Vmax≥ 99th percentile). There was a steady increase in mortality rates in Groups B-D, which an exponential increase in mortality in Group E. This pattern was also accompanied by an increasing frequency of end-organ comorbidities (dementia, chronic kidney disease, peripheral arterial disease, and heart failure) and cardiac functional and structural changes.
These results are supported by studies demonstrating that two major factors affect survival in AS: comorbidity and cardiac changes. Patients with more comorbid conditions are at a higher risk of being in conditions where supraphysiologic cardiac output is needed, placing additional stress on the already-strained heart. One of the cardiac structural changes caused by the chronic pressure overload in AS is an increase in left ventricular mass. This leads to higher filling pressure, resulting in diastolic dysfunction, which often precedes systolic dysfunction, and onset of symptoms in most patients. Traditionally, an ejection fraction (EF) < 50 per cent or symptom development have been used to define cardiac dysfunction, but these may represent later stages of AS. Because AVR has typically been restricted to symptomatic patients with severe AS, intervention in this later stage may have reduced benefit. Irreversible myocardial damage may have already been established. The results of this large study support considerations for earlier intervention in AS patients with Vmax≥ 3.2 m/sec consistent with moderate AS.
Thereafter, we developed a risk prediction model for mortality in patients with AS using a subgroup analysis of the aforementioned cohort. We calculated the risk of 1- and 5-year mortality for patients who have moderate or severe AS. The models included only patients with complete follow-up (3966 in the 1-year, and 816 in the 5-year model) and encompassed variables related to patient characteristics, degree of AS, and AVR. Amongst the 13 variables included in the final models, AVR was the strongest predictor associated with decreased mortality and improved longevity. Yet, a large fraction of patients did not undergo intervention (97.2 per cent of patients with moderate and 57 per cent of patients with severe AS). This underscores the existing gap in management of AS. In a contemporary report, 74 per cent of patients with severe AS who did not undergo AVR, were not referred for evaluation. Hence, tools such as this individualised risk calculator can help patients and providers understand the risks of mortality associated with medical management of moderate and severe AS over the short and long terms. This may eventually lead to expeditious referral to specialized centers.

On the other hand, there are currently no screening algorithms to diagnose AS, and so many patients are diagnosed later in the disease process based on symptom onset, which occurs after a long period of asymptomatic AS. As a result, there is a need to develop tools for screening programmes for earlier diagnosis. In another large crosssectional study conducted by our group, we developed an algorithm for early diagnosis of AS. Using echocardiographic results and data from the electronic health records, we developed a prediction model to identify patients with moderate and severe AS-based on readily available demographic and comorbidity information. Compared to patients with no AS, patients with moderate or severe AS were more likely to be older (mean age 76.6 ±11.3 years vs. 66.4 ±13.3 years), male, and Caucasian. They also had a higher prevalence of hypertension, dyslipidemia, coronary artery disease, pulmonary hypertension, heart block, atrial fibrillation, cerebral infarction, peripheral vascular disease, chronic kidney disease, diabetes mellitus, dementia, inability to walk, heart failure, dilated cardiomyopathy, pacemaker, defibrillator, percutaneous coronary interventions, and coronary artery bypass graft. Additionally, they were more likely to be taking beta-blockers, calcium-channel blockers, angiotensin - converting enzyme inhibitors, and diuretics. This model has the potential to be used clinically because it relies on readily available data from patient charts and is simplified to a point coring system that is translated into the probability of a patient having moderate or severe AS. Identification at the moderate stage of disease can prompt future diagnostic assessments, such as echocardiogram, with the goal of timely intervention aiming to increase survival and improve quality of life of patients with AS.
References
Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics‐2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67‐e492.
Goody, P. R., Hosen, M. R., Christmann, D., Niepmann, S. T., Zietzer, A., Adam, M., Bönner, F., Zimmer, S., Nickenig, G., & Jansen, F. (2020). Aortic Valve Stenosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 40(4), 885–900. https://doi.org/10.1161/atvbaha.119.313067
Lindman BR, Clavel MA, Mathieu P, Iung B, Lancellotti P, Otto CM, Pibarot P. Calcific aortic stenosis. Nat Rev Dis Primers. 2016 Mar 3;2:16006.
Yousef, S., Amabile, A., Huang, H., Agarwal, R., Singh, S., Ram, C., Milewski, R. K., Assi, R., Zhang, Y., Krane, M., Geirsson, A., &Vallabhajosyula, P. (2022). One and five-year mortality risk prediction in patients with moderate and severe aortic stenosis. Journal of Clinical Medicine, 11(10), 2949. https://doi.org/10.3390/jcm11102949
Lancellotti P, Magne J, Dulgheru R, et al. Outcomes of patients with asymptomatic aortic stenosis followed up in heart valve clinics. JAMA Cardiol. 2018;3(11):1060‐1068.
Yousef, S., Amabile, A., Ram, C., Singh, S., Agarwal, R., Milewski, R., Assi, R., Patel, P. A., Krane, M., Geirsson, A., &Vallabhajosyula, P. (2022). Direct relationship between transvalvular velocity and cardiac dysfunction, morbidity, and mortality in patients with aortic stenosis.
Journal of Cardiac Surgery. https://doi.org/10.1111/jocs.17199
Delesalle G, Bohbot Y, Rusinaru D, Delpierre Q, Maréchaux S, Tribouilloy C. Characteristics and prognosis of patients with moderate aortic stenosis and preserved left ventricular ejection fraction. J Am Heart Assoc. 2019;8(6):e011036.
Ozkan A, Kapadia S, Tuzcu M, Marwick TH. Assessment of left ventricular function in aortic stenosis. Nat Rev Cardiol. 2011;8(9): 494‐501.
Tang L, Gössl M, Ahmed A, et al. Contemporary Reasons and Clinical Outcomes for Patients
With Severe, Symptomatic Aortic Stenosis Not Undergoing Aortic Valve Replacement. Circ Cardiovasc Interv. 2018;11(12):e007220.doi:10.1161/CIRCINTERVENTIONS.118.007220
Yousef, S., Amabile, A., Ram, C., Huang, H., Korutla, V., Singh, S., Agarwal, R., Assi, R., Milewski, R. K., Zhang, Y., Patel, P. A., Krane, M., Geirsson, A., &Vallabhajosyula, P. (2022).
Screening tool to identify patients with advanced aortic valve stenosis. Journal of Clinical Medicine, 11(15), 4386. https://doi.org/10.3390/jcm11154386