In cases of coronary artery bypass grafting surgery for patients with multiple diseased vessels, surgeons with high multi-arterial annual volume select older patients with multiple comorbidities for multi-arterial revascularisation and achieve a better long-term survival for their patients as compared to surgeons with lower volume of multi-arterial surgeries.
The approach of coronary artery bypass graft surgery (CABG) has been changing throughout the years with regards to the type of the bypass graft used. The surgeon’s main goal is to optimise good conduit flow and long-term patency of the grafts when performing CABG surgery.

Prior literature has demonstrated that arterial grafts are superior to venous grafts in terms of angiographic patency and survival rates. Several published observational research papers have reported that arterial grafts carry longer survival rates and have better mid and long-term patency rates than saphenous vein grafts. With this available information, arterial conduits have been recommended in U.S and European guidelines and in a recent Society of Thoracic Surgeons position paper. In patients with multi-vessel disease, single arterial conduits are more commonly used than multi-arterial conduits. The reason for this is that multi-arterial grafts’ benefits are still being debated and studied in both clinical trials and retrospective observational research.
Deciding whether the patient will receive multi-arterial graft or single-arterial graft for their CABG surgery depends on several factors. The surgeon takes into account patients’ characteristics such as age, preoperative risk profile and the complexity of coronary disease.
While the use of multi-arterial graft CABG for treating patients with multi-vessel disease is recommended in recent published clinical guidelines, but statements such as "further research is needed" or "insufficient clinical trial data available" might have played a role in the decreased utilisation of this technique. Moreover, the clinical guidelines do not include specific recommendations for various clinical subgroups of patients who require CABG for multi-vessel disease. There are several other factors that account for the low rate of multi-arterial graft use, including the absence of significant evidence from large randomised clinical trials regarding survival and long-term outcomes, the surgical technical challenges, complexities involved, and the longer operative times required for multi-arterial graft surgery.
Despite the reported superiority of multi-arterial graft compared to SAG, it is still utilised in fewer than 10 per cent of coronary bypass operations in the US, with extreme variation in frequency of use between individual surgeons. A recent report from the Society of Thoracic Surgeons database showed a decline in the utilisation of multi-arterial graft CABG for all patients from 2008 to 2018 despite the reported benefits and recommendations by guideline.
To evaluate this relationship, we designed a retrospective cohort study using the mandatory New Jersey State Open Heart Registry to identify patients undergoing multi-arterial CABG between January 1, 2000 and December 31, 2016 and obtain their baseline characteristics such as age, sex, medical history, preoperative risk factors and operative information. To obtain information on the long-term survival, we linked this large database to New Jersey vital statistics death registry. The last follow-up date was December 31, 2019.
We included New Jersey residents’ patients who were diagnosed with multiple coronary vessel disease comprising males and females from different age groups, patients with diabetes, peripheral vascular disease, left ventricular dysfunction, and patients with multiple comorbidities who underwent isolated multi-vessel CABGs containing at least two arterial conduits. We excluded patients who underwent CABGs for single vessel disease, who underwent CABGs with only venous grafts or single arterial graft, patients who underwent previous heart surgeries, haemodynamic instability (pre-operative shock, cardiopulmonary resuscitation, or inotrope requirement), CABGs done in emergency settings and patients who are non-NJ residents.
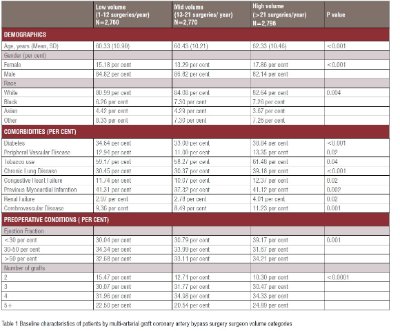
To obtain multi-arterial CABG volumes, surgeon volume was calculated as the number of multi-arterial revascularisation surgeries in the 365 days prior to the index case. Surgeon volumes were categorised into tertiles: low (1-12), mid (>12 – 21), and high (>21) volume. Low volume surgeons performed on average seven multi-arterial CABG/year, mid volume surgeons performed 17 multi-arterial CABG/year and surgeons from high volume group performed 40 multi-arterial CABG/year.
Our data constituted of 8,326 patients who underwent multi-arterial graft surgery; 2,760 (33.2 per cent) of the cases were performed by low-volume multi-arterial surgeons, 2,770 (33.3 per cent) by mid volume surgeons and 2,796 (33.6 per cent) by high volume surgeons.
Table 1 shows baseline characteristics of the patients included in the study in each surgeon multi-arterial graft volume group. There were significant differences in baseline patients’ characteristics between surgeon volume groups. Patients receiving multi-arterial grafts by high volume multi-arterial surgeons were on average two years older, had higher proportion of female patients, and patients with a higher prevalence of diabetes, peripheral vascular disease, renal failure, chronic lung disease, congestive heart failure and cerebrovascular disease, than those operated on by lower multi-arterial volume surgeons.
Patients were follow-up for 15 years. After adjusting for confounding factors (age, gender, BMI, race, comorbidities, and preoperative conditions), the hazard of death was significantly decreased by 13 per cent among patients who were treated by high-volume multi-arterial surgeons compared to mid, and low volume multi-arterial surgeons.
Our study showed significant differences in baseline patient characteristics between surgeon volume groups. Patients who were operated on by high multi-arterial graft volume surgeons were older and had more comorbidities than those operated on by lower multi-arterial volume surgeons. This finding points out at one of the important factors exploring surgeons’ preference in choosing patients for multi-arterial graft procedures. Surgeons who performed more multi-arterial graft procedures had a more aggressive approach in selecting patients for multi-arterial graft surgeries. This could mean that more training and experience is needed to select older patients and those with more comorbid conditions for multi-arterial graft procedures. This aligns with most of the descriptive baseline characteristics of patients in prior studies comparing multi-arterial graft vs single-arterial graft. A recent retrospective cohort study comparing long-term outcomes of multi-arterial vs single-arterial graft procedures showed that single-arterial CABG patients were older (mean age 68 vs. 61 years; p < 0.001) and had more comorbidities.
Naturally, having multiple comorbid conditions in patients with multivessel disease contributes to worse outcomes after CABG surgery, thus offering multi-arterial graft surgery to these patients could contribute to better outcomes. In our recently published work using the same registry, we compared long-term outcomes between multi-arterial and single-arterial procedures in 24,944 patients with diabetes. If diabetic patients underwent multi-arterial grafting, they demonstrated improved long-term survival, lower incidence of reoperations, stroke, and myocardial infarction when compared to the patients with single-arterial grafting.
The underutilisation and hesitancy to offer multi-arterial graft procedures need to be changed. It is important to explore the areas for improvement to further increase the use of multi-arterial graft procedures to improve long-term outcomes. The proposed areas of improvement from prior studies include the need of more high-quality evidence, technical skills, and rigorous training to overcome the increased complexity of multi-arterial graft procedures.
The use of mandatory large clinical registries and administrative databases produced a large sample size, thereby increasing the power of the study. Using health registries resulted in a more representative sample of the general population.
Surgeons performing a high volume of multi-arterial CABG select older and sicker patients for multi-arterial revascularisation and they achieve the better outcomes as compared to surgeons with lower volume. Despite the better outcomes, utilisation of multi-arterial procedures declined suggesting that coordinated efforts are needed to offer the multi-arterial grafts to more patients. It is necessary to educate new surgeons in this technique in order to overcome technical challenges and eliminate this practice gap.