This article will explore how virtual health is impacting in-person interactions. It will offer a different take on Telemedicine: how has equipping healthcare professionals with online consultation skills affected the classic consultation experience? How can closing the gap online improve patient engagement and health outcomes offline?

Telemedicine is by no means a new idea, but over the past few years we have seen unprecedented expansion, evolution, and a greater understanding of its potential to improve healthcare. It might be strange to discover that this impact has not been confined to the online setting but has also created ripples that impact offline care too.
Even before the pandemic, China saw the potential of telemedicine, leading to a boom in the use of virtual health services starting in 2014. This only accelerated in 2020 when the pandemic hit, creating a tipping point, changing both the way that hospitals and doctors were able to provide care, as well as how patients were able to access it. As a result, the mindsets of both physicians and patients and their behaviour towards telemedicine had to change quickly to adapt to a new era of healthcare.
Of course, this shift was felt across all aspects of healthcare, including health literacy. When the Alliance & Partnerships for Patient Innovation & Solutions (APPIS) community came together in March, their discussion around health literacy focused in on how to empower meaningful conversations between patients and healthcare providers, including in an online setting. Bringing together perspectives from different stakeholders from across the health community, including physicians, patient organisations, academics and policy makers, the in-depth discussions looked at improving online health literacy as part of a broader drive towards accelerating access for patients.
As virtual health and telemedicine have evolved, they have created new challenges around health literacy yet at the same time they have presented opportunities to improve healthcare outcomes for patients. In fact, telemedicine has created surprising, lasting improvements for both patients and physicians in three main ways: more practical training for physicians; increased health literacy for patients; and deeper relationships between patients and physicians.
As we find ourselves at another crossroads in the provision of healthcare — this time, transitioning from care that is heavily reliant on telemedicine to a hybrid era that includes both virtual and in-person interactions — we need to build on the learnings of the last few years to ensure we are giving patients access to the best care possible, no matter where that might be.
Before the pandemic, there were existing problems with in-person patient care in China. For example, Chinese physicians had limited time to see patients, as they often saw up to 80-90 in a day. At a rate this high, it was extremely difficult to provide quality care to each patient, as it meant that physicians only had a few minutes with each patient. In addition to diagnostic care, it also caused a lack of meaningful interaction or relationship, which was seen in indicators such as little to no eye contact. This kind of behaviour could lead a patient to think that the physician is not listening attentively and has little interest in the patient and what he or she has to say, diminishing the level of trust and overall patient experience.
When doctors moved onto virtual platforms during COVID-19, we saw them bring some of these familiar, bad habits to the online setting. One major cause for the ongoing issue was that many physicians did not receive proper training to provide online services for patients. To ensure physicians have the resources they need to give patients the best care possible, comprehensive training is key. As an example, our team at DXY.cn spent a lot of time training physicians through curriculums that focused on not only medical knowledge, but patient communication. This was further supplemented by peer reviews and practical hands-on scenarios with patient volunteers to make sure the training involved real-life situations. The goal of this comprehensive training is to train doctors to think beyond the illness or condition and treat the patient based on his or her individual, holistic needs.
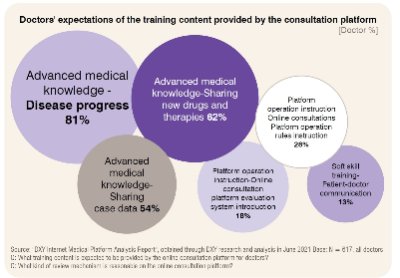
This training proved to be invaluable for virtual health consultations during COVID-19. As doctors went back to in-person consultations, we noticed a continued positive impact: the virtual training that physicians went through stuck. Physicians came back to in-person consultations with the disease education and patient communications skills to provide better service to patients compared to pre-pandemic times. Doctors also became more motivated to learn and gain knowledge, and started to expect more education from services like DXY. According to DXY’s “2021 Chinese Doctor Insight Report - Online Medical Behavior Analysis,” after conducting more online consultations in 2021, more than 80 per cent of doctors expected the platform to provide training content on advanced disease progression, sharing new drugs and therapies (62 per cent), and patient-doctor communication (13 per cent) to improve their medical skills further. As a result of their increased knowledge and training, doctors also became more willing to proactively share information with patients, with 60 per cent of doctors willing to carry out science popularisation. And through better patient communication skills, doctors delivered their knowledge in a way that patients could better understand.
More practical training for physicians had a direct impact on the patient experience in the form of more attentive care towards patients, as well as practical resources that they could use to increase their understanding of medical conditions. These resources were provided to doctors as part of the physician training at DXY. The materials, including simplified content templates, provided in-depth and practical guidance for a variety of different scenarios, covering topics from explaining diseases to patients, to educating patients on long-term care, and offering comfort for patients in difficult times.
The guidance within these materials not only proved to be valuable for physicians when working in a virtual health setting, but they also contributed to improved patient experiences offline. In addition to resources for doctors, we also provided resources for doctors to share with their patients. These digestible materials included both print-outs and QR codes that led patients to general Q&A content to learn more. We found that patients really appreciated these resources, as they helped them to better understand their health. They also strengthened the local reputations of the doctors who were providing excellent care by going above and beyond to provide as much information as possible to their patients. This was evidenced at DXY, where 99.6 per cent of patients gave a five-star rating for their physicians, and 33 per cent of patients noted that they would continue with online consultations after their first visit.
The combination of improved care from physicians and more resources provided for patients has resulted in deeper, more meaningful relationships between the two groups, in both online and offline interactions. Now that patients are going back to in-person consultations, some may have expected the number of virtual consultations to drop. However, DXY did not see a significant change in the number of virtual health visits. In 2019, the platform saw 5,000 average daily consultations. This increased to 7,000 in 2020 and dropped slightly to 6,000 in 2023. This is largely due to the fact that patients are becoming more comfortable with telemedicine when it comes to preventative medicine. For example, young mothers who are seeking general knowledge about their babies’ development are finding that their questions can be answered quickly through a virtual consultation, rather than visiting a physician in-person. There is a rising demand for people who are proactively looking for ways to improve their quality of life, rather than reactively seeking care when something is wrong.
In these cases, virtual care is seen as a source of knowledge, allowing people to quickly access the information they are looking for, without the need to travel to a clinic where they could potentially be exposed to illness.
This approach allows in-person visits to be more focused on situations around specific diseases. In cases like these, diagnostic results and physical checks are necessary to provide specific results and meaningful care to patients. Although there is always a gray area, this clearer division of online vs. offline care post-Covid has allowed doctors in both scenarios to offer more time for the patients they can help the most, allowing them to build patients’ trust. In fact, our report found that the doctor-patient interactions saw improvement in 2021, as doctors were willing to devote more time to online consultation, with 41 per cent of doctors willing to spend 10-20 minutes for a single consultation.
In the years to come, there is a huge potential for technology to continue to help physicians work effectively, while expanding access to patients in remote areas. As innovative technologies make their way to healthcare, there is an opportunity for us to embrace them. For example, Large Language Model (LLM) can help alleviate physicians’ workloads and even work as a partner or copilot by helping physicians to communicate with remote patients more efficiently. At DXY, we are already starting to use LLM to help doctors collect patients’ complaints and summarise them into a more clear and systematic information flow, so that we can use the information to provide better care for patients.
As we learn to adapt with these new and exciting technologies, we should keep in mind that while there are exciting developments happening virtually, we must ensure that more traditional, offline care is not left behind. In-person interactions will remain a critical part of delivering care to patients. Continuing to build a strong patient-physician relationship – both online and offline – will be key to ensuring that patients receive the best care possible, no matter where technology takes us!