The introduction of robotics has transformed healthcare by redefining a whole new level of surgical excellence. This impact of robotics in Orthopaedic Joint Replacement Surgeries has been nothing short of groundbreaking. Absolute surgical precision, consistency of execution, enhanced surgical efficiency and better patient outcomes are now readily attainable.
The integration of robotics into healthcare has revolutionised numerous medical fields, from rehabilitation robots, COVID Swab robots, pharmacy robots and the widely known Da Vinci Surgical Robot used primarily in urological and general surgical procedures. Orthopaedic surgery is also standing at the forefront of this transformative wave with robotics offering a whole new dimension of surgical excellence, unparalleled precision, improved patient outcomes, and enhanced surgical efficiency. (Figure 1)

Orthopaedic surgery deals with the treatment of musculoskeletal conditions, encompassing joint replacements, spinal surgeries, sports surgeries, trauma and fracture fixation surgeries. The incorporation of robotics in some of these domains has fundamentally altered the way orthopaedic procedures are performed, offering surgeons advanced tools to plan and execute surgeries with exceptional accuracy.
Robotic systems in orthopaedic surgery typically utilises advanced imaging technology, computer-aided planning, and precise intraoperative guidance. These elements work in tandem to optimise patient-specific surgical plans, streamline surgical processes, precise surgical execution, and facilitate minimally invasive techniques. This article delves into the groundbreaking impact of robotics in orthopaedic surgery especially in the field of joint replacements, examining its applications, advantages, and the promising future it holds for the field.
1.1 Preoperative Planning and Personalised Care
Robotic-assisted joint replacements have revolutionised how surgeons approach knee and hip replacement surgeries. Before the procedure, advanced imaging, such as CT scans, is employed to generate a highly detailed 3D model of the patient's joint anatomy. This has proven to be far better than the traditional 2-dimensional templating which was susceptible to inaccuracies. The comprehensive virtual representation enables surgeons to customise surgical plans according to the patient's unique joint structure, biomechanics, and individual health factors.
1.2 Real-time Feedback and precise intraoperative execution
During surgery, the robotic system serves as a virtual assistant to the surgeon, providing real-time feedback, dynamic joint balancing and ensuring the precise execution of the surgical plan. The key advantage of robotics in joint replacement surgery lies in its ability to deliver unparalleled precision and accuracy by executing movements with submillimeter accuracy, far surpassing the capabilities of human hands alone.This level of precision leads to better implant alignment, reduced soft tissue damage1, and improved joint mechanics. The minimally invasive nature of roboticassisted oint replacements results in smaller incisions, less postoperative pain, and quicker recovery times for patients.
1.3 Safety and Efficiency
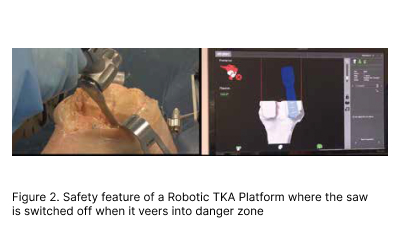
Some robotic systems employ state of the art haptic boundaries that prevent cutting tools from veering into vital neurovascular structures and therefore provide a safety check in modern robotic instrumentation. Also, with sophisticated 3-dimensional planning, implant sizes are known beforehand and this leads to improved Operating room efficiency and reduced need for cumbersome trays of heavy orthopaedic instruments. The precise guidance provided by robotic arms reduces the need for repeated corrections, thereby streamlining surgical workflows and shortening surgery duration and optimising operating room utilisation. (Figure 2)
2. Enhanced Outcomes and Patient Satisfaction
Numerous studies2 have demonstrated the superiority of robotic-assisted joint replacements compared to traditional techniques. Patients who undergo robotic-assisted procedures experience reduced postoperative pain, shorter hospital stays, and faster return to daily activities3. Additionally, improved alignment and stability of the implanted joint contribute to enhanced longterm outcomes and increased patient satisfaction4.
Through computer-aided planning, the optimal implant size and positioning are precisely determined to achieve optimal alignment and stability1. This personalised approach to joint replacements enhances the fit of the prosthesis, reduces the risk of complications, and extends the lifespan of the implant, leading to improved patient outcomes and longevity of the implant
2.1 Unicompartmental Knee arthroplasty (UKA)
(Figure 3) About 20 per cent of Osteoarthritis (OA) knees are confined to a single compartment (usually medial). A medial unicompartmental knee arthroplasty (UKA) could have been performed for this group of patients instead of TKA which is commonly performed instead. A UKA is essentially a resurfacing procedure to replace the “lost” cartilage and bone while preserving all the cruciate ligaments, which are often sacrificed in a TKA. The advantages of performing a UKA over a TKA includes a smaller incision, lesser pain, blood loss and bone resection, faster return to work and more normal knee kinematic (Figure 4)
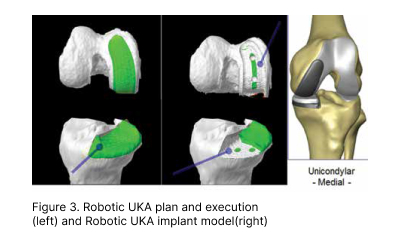

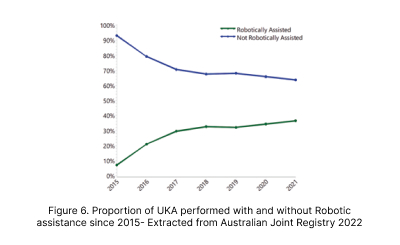
Using conventional instruments to perform UKA is susceptible to considerable alignment, rotational, sizing errors as well complications such as peri-prosthetic fractures. This has resulted in suboptimal survivorship compared to TKA data and therefore lack of confidence in surgeons to perform conventional UKA for patients with isolated unicompartmental disease, despite the obvious superior benefits for UKA. Robotic UKA has proven to be a game-changer so far, resulting in consistently accurate alignment, reproducible results, optimal implant sizing, tracking, soft tissue balancing, better forgotten joint scores (a score that measures patients’ awareness oftheir joint after a joint replacement) and lower revision rate (Figure 5).
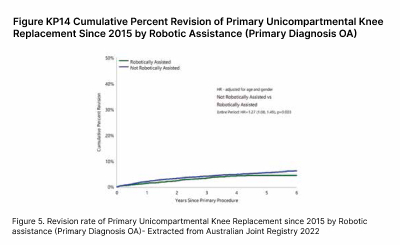
The obvious superiority in outcomes has resulted in more than 3 fold increased adoption of robotics in UKA in Australia over the past 5 years.(Figure 6)
2.2 Total Knee Arthroplasty (TKA)
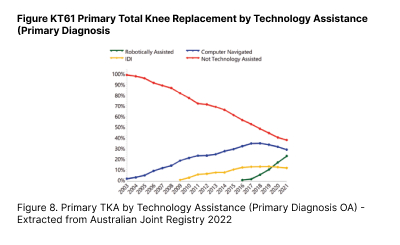
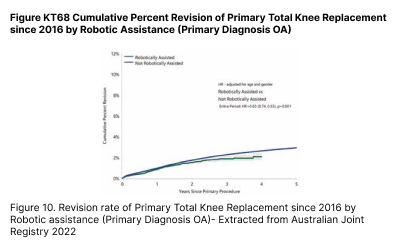
TKA is typically done for patients suffering from end stage tricompartmental osteoarthritis. In contrast to a UKA, the entire tibio-femoral compartment is replaced (figure 7). Similar to UKA, adoption of Robotic in TKA has also seen an exponential increase in Australia since its worldwide launch in 2018. In contrast, TKA done without any form of technology assistance has seen a significant drop to about 30 per cent in 2021. (Figure 8)
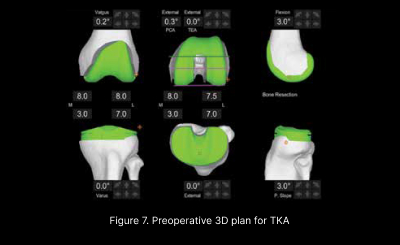
In addition to the aforementioned advantages, the precision in intraoperative execution of the preoperative plan (Figure 7) coupled with objective dynamic soft tissue balancing (Figure 9) has led to better outcomes4 and lower revision rates. (Figure 10)
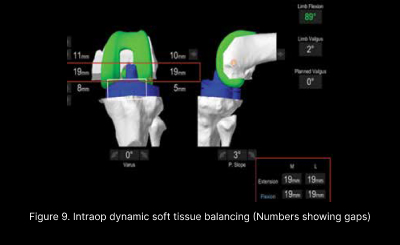
Multiple clinical studies have shown less soft tissue injury and less soft tissue releases to achieve balance therefore resulting in less postoperative pain, faster recovery and better functional outcomes3,4.
2.3 Total Hip Arthroplasty (THA)
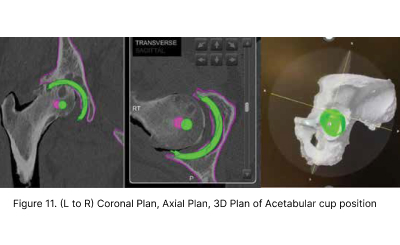
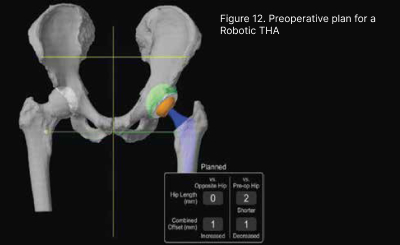
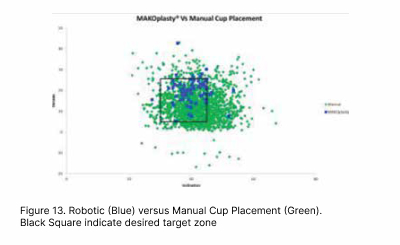
THA has been heralded as the operation of the century as it revolutionised management of elderly patients crippled with arthritis, with very good long-term results. The surgery involved replacing the damage hip joint with an artificial balland- socket joint. Robotic technology has enabled 3 Dimensional planning and precise component placement resulting in consistent and accurate acetabular cup placement compared to conventional “eyeball’ methods. This has led to lower postoperative complication rates such as dislocation and limb length discrepancy.(Figure 11 12, 13)
2.4 Complex Joint Arthroplasties
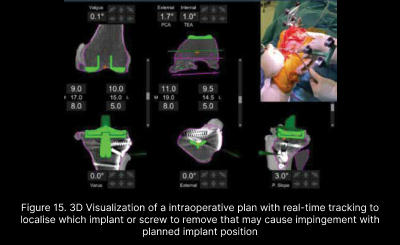
Complex Joint replacements on severe deformity or prior hardware have been simplified with the advent of robotics. Meticulous 3D planning can allow execution of well balanced joint replacement without the need for additional surgical scars to remove prior hardware as they can be largely retained without compromising optimal surgical outcome in most cases. Real time and precise intraoperative tracking can allow removal of selective hardware that may cause impingement of the planned implant position. More importantly, most of these complex surgeries can now be performed in a single stage compared to traditional methods of 2 stage surgeries, saving patients much inconvenience and costs (Figure 14, 15)

3.1 Initial Investment and Training
One of the primary challenges of integrating robotics into orthopaedic surgery is the significant initial investment required for robotic systems. The cost of acquisition, maintenance, and ongoing training can be a deterrent for some healthcare institutions. As the technology becomes more mainstream, it is expected that the costs will gradually decrease, making roboticassisted surgery more accessible to patients.
3.2 3D printing and Robotics
3D Printing coupled with robotics will bring about the next era of personalised Joint Replacements. This will make complex hip and knee surgeries even simpler and efficient, also negating the need for staged operations. This can bring about many conveniences and cost savings for patients. Presently, 3D printed implants are costly and resources are limited. In the future with improved 3D printing technology and resources, the accessibility and affordability would be better.
3.3 Advancements in Artificial Intelligence (AI) and Machine Learning
The future of robotics in orthopaedics lies in its integration with artificial intelligence (AI) and machine learning (ML). AI-powered robotic systems have the potential to learn from vast datasets, optimise surgical plans, and adapt to real-time changes in the operating room. Machine learning algorithms can analyse patient data and surgical outcomes to identify trends and improve treatment protocols continually. Moreover, AI can assist in predictive analytics, risk assessment, and personalised patient care, revolutionising the field of orthopaedics.
3.4 Telemedicine and Remote Surgery
The rise of telemedicine and remote surgical capabilities presents exciting possibilities for the future of orthopaedics. Robotic-assisted telemedicine can enable expert surgeons to perform complex procedures on patients in remote locations, improving access to specialised care and reducing healthcare disparities.
3.5 Ethical and Regulatory Considerations
The integration of robotics in healthcare raises ethical considerations, particularly regarding patient safety, data privacy, and the role of human intervention in decision-making. As robotic systems become more autonomous, defining clear guidelines and standards for their use is essential to ensure patient wellbeing and ethical practice
Furthermore, regulatory bodies must adapt to the rapidly evolving landscape of robotic-assisted surgery to provide clear guidelines and standards for approval and usage.
The integration of robotics in orthopaedic surgery marks a technological leap in patient care, surgical precision, and surgical outcomes. Robotic-assisted joint replacements have showcased the transformative potential of this technology.