Digital health has embarked on a new stage in Asia. Previously, the focus was on electronic medical record systems to improve safety, efficiency and patient experience. Now, leading providers are transforming to enable new data-driven approaches. They are using AI, remote monitoring, wearable devices and mobile apps to improve medical outcomes and patient engagement while reducing costs. While the FHIR data sharing standard has accelerated this trend, leading providers are also investing in data platforms for ease of management, data quality and advanced integration. Stella Ramette and Nana Khunlertkit from InterSystems will explain what they have learned, and how to simplify the next stage in your digital health journey.
STELLA: Artificial Intelligence (AI) and Machine Learning (ML) take the insights gained from data analytics and make them actionable with new predictive insights in real time. This is already having a positive impact on medical outcomes.
While AI is widely adopted for pathology and imaging interpretation, organisations have been slower to adopt its applications that offer the biggest potential for productivity improvements.
This is changing, however. Medical researchers like RAPIDx AI are now analysing data at scale and leveraging modern data platforms to provide insights into new and more effective treatments, provide evidence that they work, and integrate them into providers’ clinical workflows.
Let me give you a few other examples:
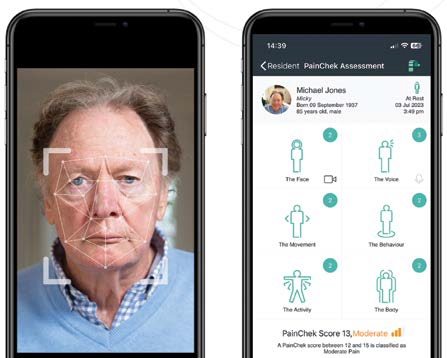
InterSystems is working with PainChek, developer of the world’s first smartphone-based pain assessment and monitoring application. PainChek’s software-as-a-service (SaaS)-based AI platform uses smart devices with cameras to evaluate patients’ pain levels accurately.
PainChek’s reliability and consistency improves care and saves time and money for healthcare providers. It also enhances the patient experience. For example, clinicians with different bedside manners may record different verbal assessments. Many patients cannot reliably describe their pain levels, are pre- or non-verbal, or are not lucid at the time.
With PainChek, a time-consuming verbal assessment and score-card process is replaced with an AI supported digital assessment and automatically generated pain rating that is more consistent and reliable than the manual process. So, you are improving care and making it more efficient. We will see more and more digital tools like this integrated into clinical workflows, which will help to relieve the workloads on our clinicians and make them more productive and effective.
InterSystems is working with another company, Cognetivity, which has developed an AI-powered test to detect dementia years before it would otherwise become noticeable. The test leverages the ‘food or fear’ response that human beings have developed about animals. Patients are shown images of animals, and an AI engine measures the accuracy and speed of responses and analyses the data to assess the patient’s risk of Alzheimer’s.
Because its solution is based on a data platform, Cognetivity has been able to rapidly integrate with existing healthcare systems at the NHS in the UK. In the early stages of adoption, this has allowed it to analyse existing demographic data to identify which patient cohorts would benefit most from being tested. It also expects to integrate with existing patient histories to perform more detailed analysis in the future. Within a short time, Cognetivity has been able to work with ten NHS trusts on research projects and implement commercial solutions at two of them.
NANA: Despite a global shortage of staff, clinicians could still misinterpret the purpose of AI as being their replacement and refuse to adopt these technologies. Successful implementations of these AI solutions have usually required strong commitment from organisation leaders, close engagement with clinicians, and a well developed change management process.

STELLA: Typically, these solutions can be made possible by integrating health data from Internet-connected devices with electronic medical record (EMR) systems capable of notifying clinicians and providing alerts.
Such approaches have been proven to work. A study at Brigham and Women’s Hospital in Boston, Massachusetts, found that remote monitoring technology improved outcomes and reduced costs by 40 per cent. Patients were also 70 per cent less likely to be readmitted.
NANA: The COVID-19 pandemic has provided a silver lining with the increased use of telemedicine, remote monitoring technology and wearable devices. And, as we discover new ways for them to support the sustainability of our healthcare systems, their importance will grow.
Telemedicine became widely used in Asia during the pandemic for urgent care, remote consultation, and following up patients with chronic conditions. Private hospitals in Thailand that were previously reliant on medical tourism, for example, switched to telemedicine to maintain a connection with their patients. More frequent telehealth follow up helped improve treatment outcomes, and lower costs have provided better value to patients.
In Singapore, COVID-19 patients were treated remotely using smartphones, tablets and Bluetooth-connected thermometers, oximeters and blood pressure meters. Hospitals in Australia also deployed monitoring devices to care for COVID-19 patients living in their homes. And in New Zealand, remote monitoring technology like ECG devices and pulse oximeters are being used to design a virtual consult service to assist vulnerable populations in South Auckland.
STELLA: Fast Healthcare Interoperability Resources (HL7® FHIR®) is not just a standardised way to share health data. It enables modern web-based technology, which was not provided by any of its predecessors, and a granular and fluid way to share and receive data. Equally important, FHIR provides curation of clean and structured data for an organisation to use for operational and clinical efficiency, analytics, mobile apps, genomics and population health. Here, the ability to ingest, cleanse and transform data is critical.
Data cleansing is not as well understood in other industries, such as retail and logistics, because typically they work with clean, real-time data. An example is a rideshare app where only real-time data about the passenger, driver and destination is managed. This is not the case with healthcare data which is complex and stored in different locations, standards and formats. To effectively make sense of the data and use it efficiently, data cleansing and harmonisation capabilities are key.
For example, there are often multiple interpretations of the same diagnosis and disparate units of measurements. One of our partners identified 58 different units strings for routine white blood cell count (WBC)! There are also several names and brands for the same drug, and multiple terms and numerical codes for a medical diagnosis. It is critical to agree on the same syntactic structure and also correct sematic data interpretation. This is the true benefit of FHIR – to enable sharing of correct information to save lives.
In Indonesia, for example, InterSystems is working with leading hospitals and hospital groups where the focus has evolved from digitisation and electronic medical record (EMR) systems to data-sharing and innovation. Many of these healthcare providers are adopting FHIR-based interoperability to integrate with other organisations, like insurance companies, or apps which enable closer patient engagement and involve patients in managing their own care.
Some are using FHIR and other advanced interoperability capabilities to integrate all of their clinical data into a single unified system. One customer has already deployed InterSystems IRIS to build a FHIR-based health data repository for operational analytics and a patient portal. We are currently working with them to ingest and analyse data at much higher speeds, enabling them to move to real-time clinical data analytics.
It is a sophisticated journey that needs to start ASAP. We see a similarity in the adoption of FHIR in healthcare and the adoption of the SWIFT international transfer standard in the banking industry. What was agreed as a standard to allow cross-border payments by 239 banks in 1973 became a universal standard.
NANA: Because of its capabilities and rapid adoption as a standard, FHIR has become recognised as the fastest and most cost-effective interoperability tool. Many governments in South East Asia are building healthcare data-sharing infrastructure based on FHIR, or encouraging healthcare providers to adopt FHIR so that they can participate in data-sharing initiatives.
Leading Asian healthcare providers are also looking to FHIR-based interoperability to further innovate by sharing between their own systems to enable data analytics, AI and machine learning, for example, to further improve quality of care, patient experience and engagement, and operational efficiency.
STELLA: Technology has advanced enormously in healthcare in recent years. We have seen a breakthrough in interoperability with the FHIR healthcare data standard. With cloud computing, we have also seen a revolution in how computer systems are deployed and scaled up to meet demand. And we have seen the advent of cloud-based data platforms, like InterSystems IRIS for Health®, that enable interoperability, data cleansing and data analysis in the cloud.
As a result, it has never been easier or more cost-effective to exchange healthcare data between different systems, ensure it is fit for purpose, and analyse it in real time. With advances in interoperability and cloud computing, AI and ML are taking off in healthcare, encapsulating the insights gained from earlier analysis to provide predictive, actionable insights in real time.
Interoperability is not the only enabling technology that data platforms need to provide for digital health. Building the infrastructure for FHIR-based interoperability is relatively easy. The more challenging part is what you do with the data when you get it. Access to patient medical records is a great starting point. But, if the data isn’t usable at the point of care, isn’t trusted, or isn’t subject to the appropriate clinical governance, it won’t make a big enough difference.
AI and machine learning algorithms enable incredible breakthroughs in the quality and cost-effectiveness of care. But if they are not clinically tested, no one will use them. If you want to see an exciting example, look at what RAPIDx AI is doing to clinically test the use of AI algorithms to improve the emergency care of people with chest pain.
NANA: A healthcare data platform enables these sorts of breakthroughs by connecting and translating health data sources, ensuring data quality, and delivering the data to where it needs to go, when it is needed. But a proven customer engagement and software implementation methodology, like InterSystems ARIES, is equally important for success.
ARIES includes five stage gates (starting from pre-sale to adoption sustainability) to ensure change management and system adoptions are properly planned and carefully executed to deliver the ‘biggest bang for the buck.’ We understand the danger of ‘garbage in, garbage out’ and, with ARIES, we design and implement a platform that will provide a clean and structured set of data, and can be easily sustained and support advanced analytics in the future.
STELLA: Healthcare providers must evaluate data platforms against several important criteria, depending on their objectives. These include:
NANA: Equally important, with all systems implementations healthcare providers need to understand that it is crucial to consider how planned workflow changes will affect staff members and take their existing mindsets into account with a well thought-out and implemented change management program.
End users do not always know what they need, although they can usually talk about what they want. As a vendor/implementer, our job is to encapsulate realistic long-term benefits to create a shared vision with the provider’s team to achieve them.
Essentially, it is to find the optimum design to fit with each provider. The optimum design does not mean endless user interface modifications to fit with end users’ expectations. But it is the most optimum design of system to be able to run operations more efficiently and effectively, and to be able to provide cleaner structured data for future analytics. With proper implementation, data management is made easy and scalable.
STELLA: The primary benefit of an advanced data platform is the ability to innovate to utilise healthcare data better. The data platform enables this by:
NANA: One solution is to improve healthcare outcomes AND reduce the cost of medical treatment. This is the idea behind value-based care. But first, you need to capture data about the effectiveness of outcomes and the cost of treatment and analyse it. A platform that allows for data sharing can improve value-based care, for example, through a reduction of care duplications among multiple providers. With an open platform, care providers can have access to more accurate, timely and complete data.
Another solution, according to Gartner, is productivity improvements from a digital-first model that breaks away from traditional in-person-centred approaches to “one that prioritises digital engagement and the use of digital products and service throughout the entirety of an individual’s health journey.”
These approaches require the healthcare industry to innovate on healthcare data management, integration and interoperability. With a healthcare data platform that supports innovation, healthcare providers are better positioned to adopt new models that support better care coordination, improve patient outcomes and reduce costs.
STELLA: Privacy is always a hot topic in healthcare, and recent data breaches have put this in the spotlight. Across all industries, information security is a significant risk, and it is a challenge that all healthcare organisations face. Healthcare data sharing through systems integration or interoperability requires organisations to conduct risk assessments and tailor their security policies and measures accordingly.
InterSystems has also invested heavily in capabilities to support robust security and privacy models within our products and partner with our customers to ensure their systems are secure. The InterSystems Global Trust program ensures the appropriate controls and measures to protect and safeguard information. InterSystems takes data security and privacy seriously and maintains a data governance framework consistent with our Data Protection, Privacy & Security Policy.
For example, InterSystems is partnering with an innovative health tech company in Singapore, Jonda Health that takes data privacy and security very seriously.
According to Dr Suhina Singh, Co-founder & CEO, Jonda Health: “Data privacy and security is at the heart of everything that we do. We believe that it is a fundamental human right. That’s why we not only use cryptographic end-to-end security but also zero-knowledge encryption. In our patient-facing application, this ensures that only patients can decrypt their data, giving them full control of their health information.
“Given we are dealing with large amounts of unstructured data, we require massive processing capabilities. As such, we are incredibly thankful to have InterSystems as a partner to help fulfil our mission. Jonda Health leverages the InterSystems IRIS® data platform to provide the scale, speed and power we need.
“The ability to share data securely without hassle is key to creating the frictionless consumer experience that patients deserve and healthcare organisations must achieve. This also promises to eliminate treatment delays, unnecessary testing, and wasted time and money.”
NANA: New digital technology also throws up many ethical issues, which play out in many industries. Thankfully, healthcare is much better positioned to respond to ethical issues than almost any other industry. Clinical governance of new treatments and technologies is not an afterthought in healthcare. It is a core competency of all clinicians and healthcare organisations. We have years of experience working with our customers to address issues when they arise and help them configure our solutions.
For example, InterSystems global partner, PainChek, has regulatory clearance as a medical device in Australia, the UK, Europe, Singapore, Canada and New Zealand and an application to the U.S. FDA is currently in progress.
NANA: In a word: innovation. No one healthcare organisation can analyse all the healthcare data that it collects. But together, as an industry, we can promote innovation and share data-based solutions that all organisations can use.
In Asia, governments see the digitisation of healthcare and interoperability to enable data sharing between healthcare providers as key building blocks for data-driven healthcare. Until recently, these governments have focussed on the digitisation of healthcare. As the number of healthcare providers with EMR and other healthcare information systems reaches critical mass, they are turning their attention to interoperability and innovation.
STELLA: Leading Asian healthcare providers are not just waiting for government-led initiatives, however. The business case for better interoperability is already becoming apparent, and the cost of providing that interoperability with standards like FHIR has never been lower.
We have also seen an innovation mindset develop around the use of data in healthcare. There is now a global ecosystem of researchers and medical start-ups pushing the boundaries in using data to improve healthcare outcomes and operational efficiencies.
InterSystems is working with start-ups around the world, including companies like RxPx, which supports the introduction and safe use of new medications with data-driven apps and systems, as well as Cognetivity, PainChek and Jonda Health, which I mentioned before.
NANA: Resourcing is always an issue in healthcare. Resources have traditionally been focussed on the areas of most acute need, like hospital care. On the other hand, precision medicine and preventative health has more potential to improve health and wellness but needs to be better resourced. The same is true for data-driven healthcare.
Healthcare organisations are constantly challenged when funding digital healthcare and resourcing projects. That limits the pace of change. There is a particular challenge in creating any system-wide business case to justify the resourcing of clinical analytics and the interoperability to support it. But that is a structural issue within healthcare systems, not a technological one.
How do we overcome this going forward? In the business world, there is the concept of a growth mindset and how that promotes cultural change and innovation and disruption to existing business models. In the healthcare sector, the equivalent idea is value-based care.
Modest investments in interoperability and analytics can enable healthcare providers to better understand the cost and the outcomes of care and provide the evidence to support changes that improve how healthcare is delivered.
Right now, that is mostly only possible within organisations or the most integrated parts of the healthcare system. But more broadly, successful value-based care initiatives can make an enormous difference, because success is contagious.
Each successful value-based care initiative provides a model and the incentive to join up other parts of the healthcare system to get further benefits and increase the number of stakeholders who get those benefits.
In other words, there is a powerful network effect, and that has the potential to move the dial significantly in the future.
NANA: As a vendor, we are committed to leading the data-driven healthcare trend. Both InterSystems products (data platform and health information systems) and our implementation teams have been built to support the future evolution of healthcare ecosystems globally and in Asia.
References:
1 https://healthtranslationsa.org.au/projects/rapidx-ai/
2 https://www.healthline.com/health-news/being-treatedat-home-can-help-people-save-money-and-heal-faster
3 https://healthtranslationsa.org.au/projects/rapidx-ai/
4 https://www.i2b2.org/
5 https://www.intersystems.com/GTDPPS
6 https://www.jonda.health/