A body of evidence has shown that an exaggerated blood pressure (BP) response to standing (BPRTS) is often present in the general population as well as in several chronic diseases and that it may be of clinical value. In recent years, evidence has accumulated that orthostatic hypertension (OH) is associated with increased risk of hypertension, hypertension mediated organ damage, cardiovascular (CV) disease and mortality. Most information on OH comes from studies performed in elderly subjects whereas much less is known about its prevalence and clinical significance in younger individuals. In this short review the available evidence regarding the prevalence, diagnosis, pathogenetic mechanisms and risk of adverse outcomes associated with OH will be presented..

A large number of different cut-offs have been used in the literature to define an exaggerated BPRTS. In the majority of the studies OH was defined as an increase of systolic BP ≥20 mmHg and/or an increase of diastolic BP ≥10 mmHg with or without including absolute values of standing BP. The prevalence of this condition proved to be much larger in elderly individuals than in younger subjects. The highest prevalence was found in the elderly participants of the PARTAGE study (28 per cent) and the lowest in a study by Wu et al (1.1 per cent). Very low prevalence was found in young people.
Other authors used lower systolic BP cut-offs to identify people with BPRTS ranging from 5 to 15 mmHg or included orthostatic BP in the definition. In a document of the American Autonomic Society and the Japanese Society of Hypertension OH was defined as an orthostatic systolic BP increase ≥ 20 mmHg associated with a systolic BP ≥ 140 mmHg on standing.
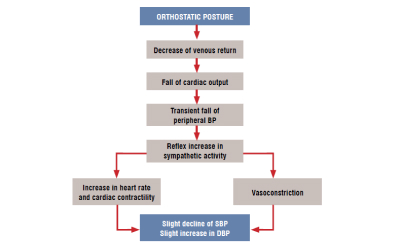
Assuming asupright posture triggers a sequence of hemodynamic changes that prevent a fall in peripheral BP (figure). On average, the final result is a slight decline of systolic BP and a slight increase in diastolic BP. However, in some individuals, the compensatory mechanisms may lead to an exaggerated BPRTS. There is general agreement that the mechanisms leading to OH may be influenced by age. Cardiovascular hyperreactivity seems to be the main mechanism in young adults and vascular stiffness the driving factor in older individuals. People with high BPRTS may have normal sympathetic activity at rest but increased sympathetic response to stressful stimuli. Previous research has shown that plasma catecholamines may increase dramatically after standing up. In the HARVEST study, hyperreactors to standing had a pronounced increase in 24-hour epinephrine urinary output. Sympathetic predominance has been found to be involved in the pathogenesis of OH also in children. Although arterial stiffness is considered the most important contributor to OH in the elderly, also baroreflex dysregulation and increased sympathetic discharge can be important determinants of OH in this age class. In summary, the pathogenesis of exaggerated BPRTS is multifactorial and our knowledge about the mechanisms involved is still incomplete.
To have a reliable estimate of BPRTS, BP should be measured starting one minute after standing up and at least three BP readings should be obtained after assuming the upright posture. In one study BPRTS was calculated using the average of the second and third measurements. Due to the limited reproducibility of BPRTS current guidelines recommend repeated orthostatic BP assessment on a different day. For screening purposes, seated to standing position can be used to assess BPRTS. However, BPRTS may be less pronounced when using seated BP and thus in subjects with suspected OH a more reliable diagnosis can be made using supine to standing measurement.
The reproducibility of OH has been found to be limited. Hoshide et al. compared the reproducibility of OH identified with clinic versus home BP. Using home BP, the concordance in the definition of OH was good with a K coefficient ranging from 0.42 to 0.51. The agreement for OH identified by clinic BP ranged between 0.13 and 0.24. A better reproducibility of BPRTS evaluated with office BP measurement was found by others within short between-measurement periods (10 to 34 days) with intraclass correlation coefficients of 0.70 to 0.86. In the Hypertension and Ambulatory Recording Venetia Study (HARVEST) the correlation coefficients between the orthostatic changes measured at baseline and after 3 months were 0.29 (p<0.001) for both systolic and diastolic BPs. The reproducibility of OH has been found to be very poor when BPRTS was re-measured after a long time interval. However, in the SPRINT trial, a fairly good concordance was found between OH measured at baseline and OH assessed 3 years later.
High activity of the sympathetic nervous system and/or baroreflex dysregulation, such as in the elderly, diabetes, and essential hypertension, are often associated with OH. In elderly subjects, diabetes is more common in patients with OH than in subjects with normal orthostatic BP. An association with obesity and metabolic risk factors has been observed either in diabetic or non diabetic subjects. Chronic kidney disease and inflammatory biomarkers are other factors that have been found to be associated with OH. In a recent analysis of the HARVEST it was found that a higher office BP and a greater BP decline during supine BP measurements were predictors of a lower BPRTS.
An exaggerated BPRTS can be a predictor of masked hypertension and as well as of sustained hypertension. Hyperreactivity to standing has been found to be associated with masked hypertension in several studies. A cross-sectional investigation performed with home BP measurement has demonstrated that OH is an independent predictor of masked hypertension. In another cross-sectional study in a general population assessed with ambulatory BP monitoring, the frequency of masked hypertension was significantly greater in subjects who showed a BPRTS >10 mmHg. Analyses of the HARVEST study have shown that baseline BPRTS was associated with masked hypertension assessed after 3 months. The risk of masked hypertension was quadrupled for the group of hyperreactors with high urinary epinephrine compared to the normoreactors with low epinephrine.
An increased risk of office hypertension was shown in the ARIC study and in the young participants from the CARDIA study but not in the Normative Aging Study, after controlling for sitting levels of systolic and diastolic BPs.
The relationship between OH and hypertension may be due to an increased large artery stiffness in people with exaggerated BPRTS especially in elderly subjects. In a multiple regression analysis the orthostatic change in systolic BP was significantly and positively correlated with pulse wave velocity in hypertensive patients whereas no association was observed in non hypertensive subjects. An association between orthostatic BP changes and large artery stiffness was found also in young and middle-aged adults.
Several studies such as the ARIC, the Normative Aging, and the PARTAGE studies have shown that OH is associated with increased risk of coronary events and stroke. In a large Chinese cross-sectional communitybased study, both OH and orthostatic hypotension were associated with stroke and peripheral vascular involvement. In the SPRINT (Systolic Blood Pressure Intervention Trial), an association of OH with a composite CV outcome was found within the intensive treatment group. Recent research from the HARVEST study has shown that an association of OH with CV events may be present also in young individuals.
An independent association of OH with mortality has been found in several studies which included mainly elderly subjects. However negative data have been reported by other investigators. Inconsistencies in methodology and different characteristics of the studied populations may partly explain these conflicting results.

Hypertension guidelines recommend measuring BP on standing only in elderly subjects to prevent the possible detrimental effects of orthostatic hypotension. The increased risk of developing organ damage and CV events in people with OH suggests that BP should be measured in the upright posture also in young individuals with the main aim of detecting a possible exaggerated BPRTS. BP on standing should be measured especially in people with borderline values of office BP in the sitting posture who are more at risk of masked hypertension and OH. Ambulatory BP monitoring data may be acquired to have a more detailed picture of the BP changes during standing. If high average 24-hour BP and/or abnormalities of the diurnal BP rhythm are detected, close follow-up with repeated visits should be implemented and antihypertensive treatment may be considered.
Whether a specific antihypertensive treatment should be used in hypertensive patients with OH is not known because no randomised clinical trial has been performed. Treatment with alpha blockers has provided encouraging results, but the lack of definite evidence suggests that subjects with OH should receive the same classes of drug as any other hypertensive patient.
Studies on the clinical and prognostic significance of OH have often been inconsistent due to methodological heterogeneity in definition and diagnosis. The large majority of studies have used systolic BP in evaluating the clinical significance of BPRTS but also diastolic BP reactivity has been investigated often leading to conflicting results. Future research should address the issue of appropriate definitions of BPRST and OH for different age groups.